Essential Best Practices for Verifying Insurance Every Medical Clinic Needs
Proper, error-free medical insurance verification is vital for both patients and practices. According to the latest data, about 92 percent of Americans have insurance for all or part of the year. That means a vast majority of patients coming through your practice will use their coverage to pay for at least part of their care.
An inefficient insurance verification process can be a nightmare for practices like yours, resulting in unpredictable cash flow, errors that require considerable time fixing, frequent claims denials and a host of other headaches. For patients, verification mistakes and delays can result in surprise bills that erode trust.
Insurance verification mistakes are more common than you might think.
According to a survey by Experian, 56 percent of provider respondents said that errors are a primary cause of denied claims. Those mistakes are disrupting revenue cycles and costing the industry billions of dollars annually. Practices reportedly lose up to 5 percent of net patient revenue due to errors, with some studies saying that improper healthcare insurance verification costs practices up to $25,000 per physician annually.
With errors causing delays, increased administrative burden and negative impacts to revenue cycles, more and more practices are seeking better ways to verify patient insurance. In this blog, we'll explore insurance verification best practices that make a difference, helping you handle this all-important administrative task more efficiently than ever.
Why Medical Insurance Verification is Critical for Your Practice's Success
Financially, poor medical practice insurance verification has a significant impact. As mentioned earlier, errors are a leading cause of claims denials, and the healthcare industry loses billions of dollars annually dealing with them. Larger health organizations incur losses of as much as $5 million in revenue each year due to denials and the increased administrative costs of trying to fix them. Studies suggest that the cost of reworking a single claim can cost practices anywhere from $25 to over $100. Not only that, but mistakes can delay payment by as much as 90 days, creating unpredictable cash flow for your practice.
The average practice spends more than 12 minutes manually verifying patient insurance, amounting to hours of monotonous work for a day's worth of patients. That's not considering the time it takes to chase mistakes and correct them.
Not only are there additional costs, wasted revenue and increased administrative burden, but patients suffer, too. With a majority of Americans worried about healthcare costs, surprise bills and delays caused by clunky insurance verification processes can cause patient satisfaction scores to plummet. Those issues that can then lead to low collection, retention and referral rates, ultimately affecting your practice's reputation. The consequences of inefficient processes and insurance verification mistakes are monumental, hindering your practice's path to success.
The Complete Patient Eligibility Verification Process Step-by-Step
Healthcare insurance verification workflows can vary, but a standard process will begin as soon as a patient schedules an appointment.
1. Collect Demographic and Insurance Information: When scheduling appointments with patients, collect the basics. You'll need demographics information, contact details and a photo of the patient's insurance card. Confirm policy numbers, group numbers, etc. Collecting this data as early as possible will allow you to verify patient insurance long before their appointment.
2. Confirm Policy Status and Coverage Details: Run initial checks to confirm coverage. Use payer portals to check effective dates for policy benefits, plan type, in-network status, copay, coinsurance, deductibles and more.
3. Check Treatment Eligibility: Verify coverage for planned services. Check eligibility at the CPT code level via payer phone calls. Run verification early to ensure that policies cover intended treatments. Handling this process early will give your practice ample time to contact patients if any issues arise.
4. Identify Pre-Authorizations: Remember to check for any restrictions or pre-authorization requirements. If the policy requires pre-authorization, submit requests as soon as possible. Routine approvals can take up to two weeks, with more complex procedures taking up to a month. Handle submissions early on to prevent delays.
5. Ongoing Patient Eligibility Verification: In the 48 to 72 hours before any patient's appointment, go through the medical insurance verification process again to confirm eligibility. Running an additional check before an appointment will help ensure accuracy, preventing mistakes that could result in denials. At this time, create fee estimates and confirm patient payment responsibilities.
6. Check-In Verification: During patient check-in, ensure that authorizations aren't expired, collect payment methods to prevent collection delays and communicate with patients about their responsibilities.
Advanced Verification Process Strategies That Reduce Errors
Even with a strong workflow, insurance verification mistakes can happen. Here are several strategies to mitigate the risk of errors and ensure smooth sailing for staff and patients.
• Invest in Automation Tools: Consider using verification software that can automate this process. Verification software can run checks in minutes, pulling data from payer portals. These tools can reduce staff workload and prevent the creation of redundant data. They can also flag you to potential issues that may result in claim denials.
• Integrate Tools Into Existing Systems: Integrate your tools with your EHR and practice management systems. Doing so will minimize errors caused by manual data entry while ensuring data consistency between systems.
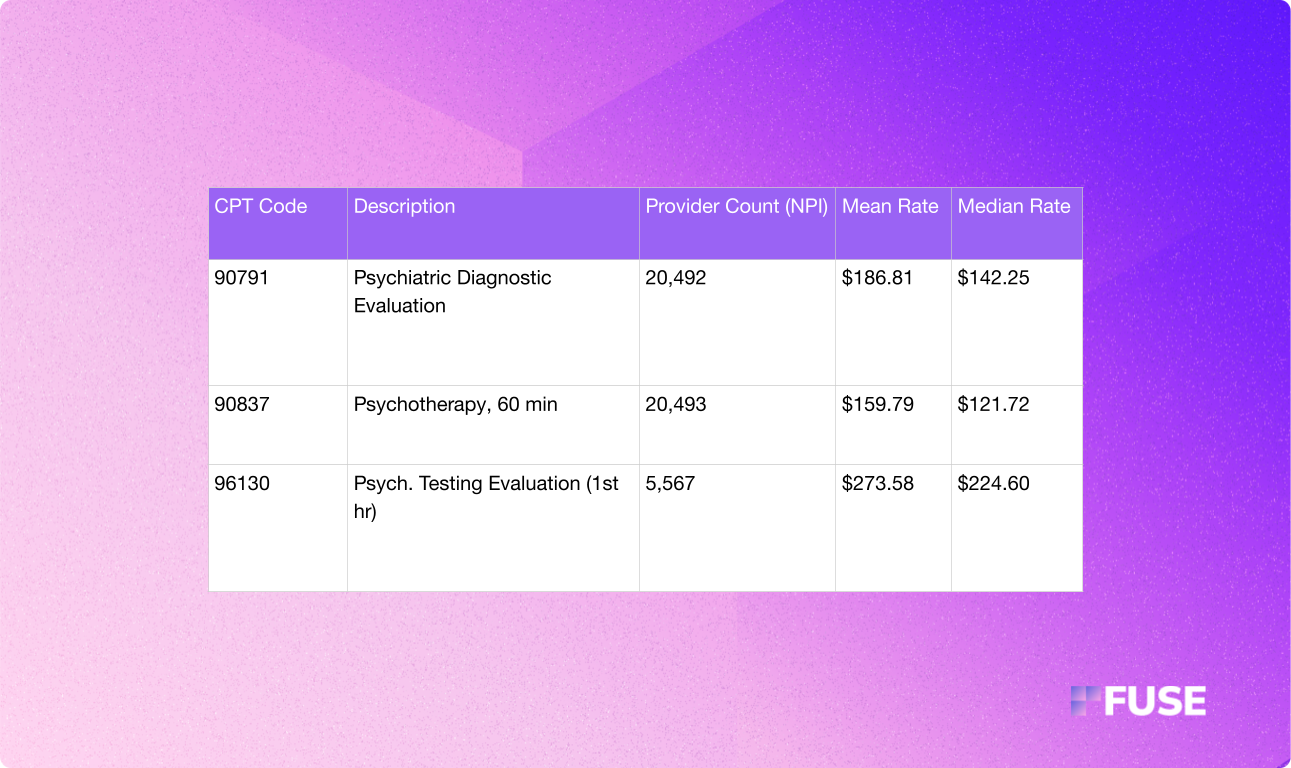
• Combine Verification Methods: State-of-the-art insurance verification processes pair payer portal checks with phone calls. Healthcare clearinghouse platforms and your EHR's portal offer quick confirmation, but they won't provide granular benefits data. To get that, you must call payers directly. Use both methods to avoid surprises and understand eligibility at the CPT code level.
• Document Everything: Record call details, save eligibility responses in patient records or billing systems, document key benefits details and standardize file naming structures. You want strong and consistent documentation to create a clear audit trail that you can reference should issues arise later.
• Train and Cross-Train Staff: Always spend time training and cross-training your staff. Teach your team how to use tools and software solutions. Ensure everyone can perform eligibility checks to prevent dependence on a single person, and monitor performance by tracking metrics to address skills gaps that could impact your insurance verification process.
How to Verify Patient Insurance Coverage Accurately Every Time
Maintaining accuracy as you verify patient insurance coverage is about asking the right questions. Whether using a portal or calling insurers directly, always begin by confirming the patient's plan status, effective dates and in-network eligibility. Verifying these details can help prevent denied claims from the jump. From there, you can dive into more information about a patient's financial responsibilities. Inquire about copays, coinsurance and deductibles. Confirm the amounts and deductible status to help patients understand what they need to pay out of pocket.
To understand pre-authorization requirements, call payers directly. Verify coverage at the CPT code level to learn about requirements like referrals, visit limits and authorization thresholds. Here are a few targeted questions to ask:
• Is this CPT code covered by the patient's policy?
• Are there any prior authorizations or referrals required?
• Does the patient's policy have coverage limitations for this CPT code or provider type?
• What are the patient's estimated financial responsibilities for this visit?
As always, be meticulous about documenting responses. Documentation should include the date of the verification, the name of the representative you spoke with, reference numbers and any other relevant details for auditing. Record a summary of coverage benefits, including specific authorizations and patient responsibilities. Save those records in your billing system or the patient's EHR for easy reference.
Common Healthcare Insurance Verification Mistakes to Avoid
Insurance verification mistakes are common and can happen to even the most well-trained staff. Fine-tuning your process and adopting insurance verification best practices goes a long way. However, you should also train your team to avoid the following mistakes:
• Waiting Until the Last Minute: Don't wait until check-in to verify patient insurance. Verification should occur as soon as possible. Perform patient eligibility as soon as possible after setting an appointment. At the latest, aim to complete verification 48 to 72 hours before a scheduled visit.
• Missing Information: Incomplete data will create delays during the insurance verification process. Collect all relevant data, including everything on a patient's insurance card, and ensure patients complete forms in their entirety. Store that data in billing and EHR systems for easy reference.
• Incomplete Verification: Your practice needs comprehensive information about a patient's coverage and eligibility. Create a standardized verification checklist for every patient, reminding staff to collect everything from coverage details to plan status and deductibles.
• Weak Documentation: Failing to record responses and reference numbers during the verification process can result in incorrect information and a nonexistent audit trail. Standardize verification documentation and immediately log records in the EHR.
•Assuming Coverage: Don't assume that patients have coverage for a service. Always perform CPT code-level checks, especially for high-risk treatments or procedures, to understand specific limitations, authorization requirements and more.
• Using Only Payer Portals: Relying solely on payer portals will leave out critical information. You must call payers over the phone to get specific coverage details at the CPT code level.
• Ignoring Secondary Coverage: Overlooking secondary coverage may result in partial payments, unnecessary delays and collection challenges. Always ask about additional coverage and perform all necessary verifications.
Maintaining accuracy should be a top priority. Standardize your insurance verification process and create a checklist for staff to use, ensuring everyone gathers all necessary information. It's also a good idea to verify at various points, including after scheduling an appointment, several days before a patient's visit and during check-in. Doing so will allow teams to double-check information for accuracy, preventing errors that could cost your practice. Finally, perform regular audits to review efficiency and quality.
Medical Practice Verification Technology Solutions
Fortunately, you no longer have to rely on manual insurance verification processes. There are many great tech solutions available that can accelerate the process, all while saving time and minimizing the risk of errors.
Automated verification systems streamline the process by checking patient eligibility and benefits against payer databases. Real-time eligibility tools are also available, providing instant access to insurance information to confirm coverage before rendering services. Software solutions that integrate with practice management and EHR systems take things further, ensuring seamless data flow and propagation. Integration can reduce manual data entry errors and duplicate information, enhancing overall workflow efficiency.
Insurance eligibility software can revolutionize your practice's entire approach. Manual approaches are time-intensive and costly. Meanwhile, automated verification can take mere minutes and cost far less. When you consider the costs and time involved with correcting errors and dealing with claims denials, the benefits of adopting tech solutions are undeniable.
Best of all, practices of all sizes have much to gain. Smaller practices can recoup the costs of implementation within the first few months. Larger practices benefit from scalability, gaining the ability to verify insurance for a high volume of patients without additional investments in staff, resulting in a significant ROI.
Transform Your Revenue Cycle with Streamlined Insurance Verification
Improving your insurance verification process can benefit your practice in countless ways. But more importantly, it paves the way to a far better patient experience. Patients already have anxieties about paying for healthcare, with many delaying it entirely due to worries about the financial side of receiving care. When you follow insurance verification best practices and streamline your practice's approach, you can put those worries to rest. It's a way to offer transparency and peace of mind to patients, which will lead to great success for your practice.
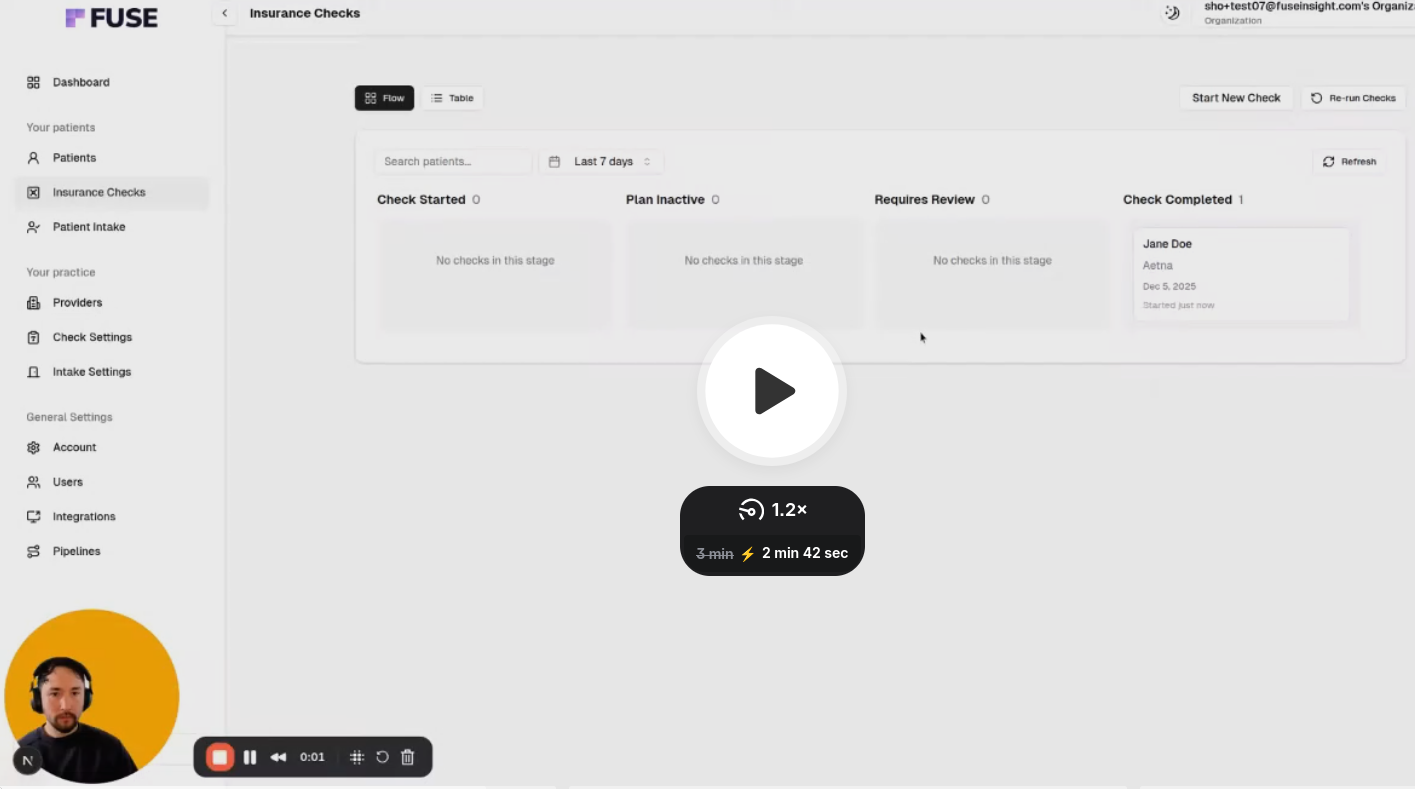
When you want to make positive changes that benefit your patients, check out Fuse. Fuse is a healthcare software solution that can automate patient insurance verification, performing CPT code-level checks quickly and efficiently. Fuse can do the heavy lifting, improving practice operations and staff efficiency while reducing denials, facilitating faster payments and increasing patient satisfaction.
Schedule your Fuse demo and consultation today to see automated insurance verification in action and discover the many ways it can transform your practice.




.avif)
.avif)
.avif)

.avif)
.avif)


