How to Create a Fuse Account and Run your First Insurance Check

In 2021, two widely used healthcare platforms, Kareo and PatientPop, merged and rebranded as Tebra. Tebra serves roughly 42,000 practices across the United States. The merger and creation of Tebra promised to streamline both clinical operations and practice growth into one, unified platform.
However, user reviews reveal major gaps between expectations and real-world performance. While the promise of fewer systems to manage, tighter integrations and enhanced operational efficiency felt like a game-changer for many practices, the reality highlights genuine issues you should know about.
Understanding real healthcare software complaints helps practices make more informed decisions about management software like Kareo/Tebra.
This analysis will cover actual feedback and verified reviews from real users across multiple platforms. We aim to provide an honest assessment, revealing genuine Kareo/Tebra complaints based on documented user experiences.
The Merger Effect: When Kareo Became Tebra
Before 2021, Kareo and PatientPop operated independently. The former was best known for its EHR, practice management and medical billing tools. Meanwhile, the latter was a popular platform for marketing, website development and patient acquisition. The two platforms officially merged in 2021 and rebranded as Tebra, combining patient management, billing and patient engagement into a single, end-to-end platform.
On paper, the merger made sense. Unfortunately, users frequently suggest that the transition created instability rather than improvement. Many report that the new instability negatively impacted practice workflows, citing system changes, new processes and unexpected feature limitations.
In verified feedback, one user mentioned a notable decline after the merge, noting they were "bought out twice," which resulted in greater instability. Some users also reported how they loved Kareo before Tebra took over, but experienced substantial problems after the transition.
One specific complaint mentioned in Tebra reviews is the visual changes. The shift in overall format and color schemes made the adjustment more difficult for users who relied heavily on color for navigation.
Customer Service Complaints Dominate User Reviews
The Kareo/Tebra complaints go beyond instability and design changes. Tebra customer service issues are a common thread in verified reviews. Many practices report that reaching support staff has become more difficult since the transition to Tebra, with one review specifically noting this was not the case early on.
Common concerns include lengthy wait times of 25 to 40 minutes to reach a customer service specialist, only to be brushed off or redirected without a resolution. Users also describe limited transparency about enrollment processes and difficulty getting answers for more complex issues. Tebra support staff reportedly sticks to the basics, which is presenting problems for practices.
Tebra customer service issues and poor EHR customer support even reached the Better Business Bureau (BBB). There are BBB complaints about delayed responses, lackluster communication and a general lack of accountability and responsibility.
One practice mentioned waiting two weeks for simple cost information during a critical transition period. These complaints are a stark contrast to early experiences with Kareo. Many users note that, before the merge, Kareo EHR customer support was knowledgeable and quick to fix issues.
Response Time Issues and Support Quality Concerns
Users frequently cite lengthy response times as a major frustration when working with Tebra customer support members. Several Tebra reviews mention that practices have to wait several weeks for a response, leaving staff without guidance during time-sensitive operational issues. In one review, the user noted that a support operator acknowledged the team was 8 to 9 days behind in responding to requests within the system.
While the company has offices in California, the support team appears to be offshore in Costa Rica. That offshore support reportedly takes over a week or more to respond to website changes. But that's not all.
As if those delays weren't enough, some reviews go into detail about the shocking responses they receive. Complaints mentioned being told to "figure it out yourself" or "suck it up." Longtime users state that support no longer pays attention to reported bugs, ignoring them outright.
The decline in quality and timeliness is proving to be a significant source of frustration for users, with many Kareo/Tebra complaints mentioning lengthy timelines and unhelpful support.
Training and Onboarding Experience Varies Widely
The onboarding and training process is critical to a practice's success, ultimately shaping their experience with the platform. User feedback for training is mixed. Some reference positive experiences with knowledgeable training managers who offer step-by-step guidance, weekly calls and comprehensive education. However, others are the complete opposite, creating many persistent practice management software issues.
Kareo/Tebra complaints mention trainers doing no more than a single session before abandoning new users. These reviews state they never hear from their trainer ever again. Some users, frustrated with the poor onboarding experience, are told to look things up online, even though they've already gone through those steps after the trainer abandoned them.
This inconsistency is problematic. There's considerable contrast: some praise Tebra's great training experience, while others struggle with zero support. For a platform that's so integral to everyday operations and growth, the lack of consistency creates a spectrum of experiences with Tebra. Those who receive adequate training and onboarding often find the software user-friendly. On the other hand, those who don't struggle with the steep learning curve.
Data Export and Vendor Lock-In Concerns
Data portability is a common complaint in Tebra reviews. Many reviews report that exporting client data from Tebra can be costly and cumbersome. Tebra reportedly doesn't allow users to export client databases in a format that other EMRs don't support. To do so, Tebra purportedly charges a whopping $2,000.
These limitations create a vendor lock-in situation. Switching platforms becomes expensive and complicated. Practices feel trapped. They face practice management software issues they no longer want to deal with, but the costs and headaches of exporting databases prevent them from migrating to another platform. Those data export challenges, paired with customer service quality issues, only compound the frustration.
Technical Issues and Software Stability Problems
According to many Tebra reviews, ongoing technical glitches are impacting everyday operations, costing practices time, money and patients. Common issues include billing errors, system outages and calendar problems. For example, some users report that the software doesn't reflect changes, such as cancelled appointments. Furthermore, new scheduled appointments sometimes don't appear in the system unless staff make repeated attempts.
Many Kareo/Tebra complaints mention overall buggy software. One reviewer went so far as to state that Kareo knew about the existing problems, saw what was happening and could not/would not do anything to fix it. They called it yet another "Kareo glitch."
Clearinghouse issues also exist. Some users complain that the clearinghouse is so unreliable that they've resorted to handling billing tasks directly through insurance portals, all to ensure claims are processed. Additional issues include frequent AWS outages that cause service disruptions and recurring EPCS vendor issues that impact electronic prescription orders.
Billing and Claims Processing Challenges
As with other practice management software issues, there are mixed reviews of billing. On the one hand, some users found Tebra's billing features to be sufficient. Some mention that billing works just fine. However, others experience excessive issues. Several reviewers call Tebra a truly terrible billing platform with poor customer service.
Frequent Kareo/Tebra complaints center on the electronic remittance advance (ERA) not always being processed through the clearinghouse, resulting in delayed payments and additional administrative work. Unfortunately, when those billing issues arise, users face the same Tebra customer service issues we mentioned earlier. That includes excessive response times that ultimately cost practices.
Like many other facets of Tebra, there's a learning curve to the billing features. Some practices manage to operate them efficiently once acclimated. However, others found that successful billing requires a workaround and direct portal access to process claims. These mixed experiences only highlight one of the most common healthcare software complaints: inconsistent performance.
Calendar and Scheduling Functionality Gaps
A functional calendar that syncs in real-time is crucial for maintaining smooth operations. Yet, several Kareo/Tebra complaints reference calendar limitations. Practices report that scheduling more than 10 appointments at a time can be cumbersome, as there's no way to view upcoming appointments without manual review.
Appointments reportedly default to a single service type. Pair that with a lack of mobile friendliness, and staff often struggle to manage even a simple task, such as setting an appointment.
Calendar features should be a home run for practice management software, helping practices streamline their scheduling. However, Tebra reviews state that limitations disrupt scheduling workflows and create unnecessary manual work for administrative teams.
Website and SEO Service Disappointments
Many Kareo/Tebra complaints highlight issues transitioning websites from the former PatientPop platform. A complaint filed with the BBB said the process takes 2 to 3 times as long as it did when PatientPop operated independently. The user reportedly experienced nothing but problems since the merger. The reviewer reported that it was next to impossible to get a hold of anyone who could help. They never resolved the issue, and the user had to pay another company $11,000 to create a new website for their practice.
Tebra also reportedly does nothing to help websites gain traffic. SEO and promotion are nonexistent according to several verified reviews, despite Tebra stating they would help promote practice websites. The drop-off in quality is noticeable. According to one user, PatientPop made more sense and was "awesome" to use 3 years ago. However, since PatientPop and Kareo merged into Tebra, that's no longer the case.
Yet again, inconsistency seems to be a significant concern. Some Tebra reviews say the platform increased website visibility on major search engines and generated a strong online presence that translated into more patients. Meanwhile, others have nothing positive to say about their experiences.
Payment Processing and Med Spa Service Restrictions
We've already mentioned practice management software issues concerning billing. Unfortunately, it doesn't end there. Some users report being unable to use Tebra Payments at all because it lacks support for certain specialty services. For example, some reviewers say they're unable to process payments because they offer Med Spa services. According to Tebra's policy, the platform won't process debit or credit card transactions for Med Spas.
Those restrictions create problems for certain types of practices. Any practice offering services outside traditional medical scopes may find payment processing incompatible. Some Kareo/Tebra complaints say that those terms weren't clear during the sales process, leading to functionality gaps after onboarding. With the high fees and migration hurdles, many practices are stuck.
Sales Process and Expectation Misalignment
For some users, healthcare software complaints revolve around sales tactics and the stark gap between expectations, promises and the harsh realities of using Tebra. Some reviewers accuse Tebra of using misleading sales strategies and communications. Sales teams allegedly offered them a product that's simply not compatible with their practice and business.
Some reviews discovered those incompatibilities and complications long after committing to and paying for Tebra. As a result, they had no choice but to find workarounds as they learned to use the software hands-on. Several reviewers mention feeling deceived by exaggerated claims.
Others find that the software doesn't live up to the promises of coding API or integrating with other systems. Instead, the platform feels outdated. If considering Tebra or any other healthcare software, it's important to do more than look for a list of features you want. Practices should thoroughly test actual workflows during evaluation to ensure platforms meet the mark.
What Works Well: Positive User Feedback
It's not all negative. While complaints about Kareo/Tebra are common, there are plenty of verified reviews that tout many positive aspects of the platform. For example, some report that Tebra is the easiest EMR they have worked on in decades, praising the software's user-friendliness, easy navigation, patient messaging capabilities and streamlined scheduling.
Users also applaud the ability to generate customized reports, the availability of a mobile app and integrated telehealth, which helps practices reduce no-shows. Tebra also gains a point for pricing transparency. Several reviews commend the easy-to-find pricing information and flexible plan options for growing practices.
While there are many Tebra customer service issues you can't ignore, some users found the support teams helpful. When support works well, and users connect with knowledgeable staff, they note how quickly they receive responses and solutions.
Ultimately, experiences vary wildly based on practice needs, specialty, implementation timing, support quality received and other relevant factors.
Consider Alternatives That Specialize In Your Biggest Pain Points
Kareo/Tebra complaints document a pattern of issues with the quality and reliability of customer support, data portability, technical stability and specialty limitations. While every experience is different, we can't ignore verified reviews from real users operating functional medical practices that rely on software like Tebra. Practices must carefully evaluate whether all-in-one platforms like Tebra truly meet their specific needs. In many cases, specialized solutions are a better option for addressing critical workflows.
Reach out to Fuse today to learn more, discuss your practice needs and discover whether specialized tools like Fuse can complement or replace your all-in-one systems.
Why Medical Practices Are Complaining About Kareo/Tebra: A Deep Dive Into User Reviews
Patient engagement has the potential to transform how healthcare practices like yours connect with patients. Automated drip campaigns in healthcare, powered by EHR data, can deliver timely, personalized messages to each patient. These messages can include appointment reminders, post-procedure follow-ups, medication adherence messages, preventative care education and much more. Best of all, powerful patient communication automation could maintain engagement without burdening your administrative team with manual work.
In theory, this type of automation is a game-changer that can save time, boost patient satisfaction, reduce missed appointments and improve overall outcomes. However, in reality, many technical barriers prevent practices from leveraging the potential of EHR data automation to achieve the seamless, hands-off workflow they want.
In this blog, we'll explore some of the most common roadblocks that prevent practices from realizing the benefits of automated EHR-driven drip campaigns and offer proven workarounds.
The Value of EHR-Driven Patient Communication Automation
When done correctly, EHR-triggered drip campaigns offer practices far more than simple convenience. They can deliver measurable results, helping engage patients better than standard marketing campaigns.
EHR-driven healthcare marketing automation delivers relevant messaging at the right time, all by using real-time patient information. That timely, personalized outreach makes a difference. Not only do messaging campaigns resonate more with patients to boost engagement between visits, but targeted drip campaigns can also reduce no-shows, improve patient education and create a more personalized experience.
That's not just hearsay. Automated drip campaigns in healthcare that use EHR data consistently outperform generic outreach. One study found that drip campaigns can achieve conversion rates of over 60 percent. Another found that drip campaigns in healthcare achieve a significantly higher click-through rate than standard emails.
Common EHR Data Automation Roadblocks Practices Face
Several technical roadblocks prevent practices from successfully using EHR data for patient communication automation. One of the biggest is the fragmented EHR landscape. There are over 600 different EHR systems in the United States, each with its own data formats, standards and coding conventions.
Data standardization issues create EHR integration challenges, as different facilities can use different codes for the same information. What one system labels as a "routine checkup" could be entirely different in another, making it difficult to establish consistent triggers for automated drip campaigns in healthcare.
Interoperability gaps add further complications. Many EHRs simply aren't built to share data freely across platforms. In fact, most legacy EHRs were purpose-built for billing. Thus, they have zero marketing integration capabilities.
Another problem is extracting data from clinical notes. Data is often unstructured, especially in older systems, making extraction both time-consuming and technically challenging.
These technical barriers turn what should be a simple, automated process into a massive headache. EHR integration challenges create risks. A lack of reliable integration and data standardization could result in inaccurate, incomplete and untimely messaging, undermining patient engagement and eroding trust.
Data Integration and Interoperability Challenges
Successful healthcare marketing automation with EHR data requires seamless data exchange. The problem, however, is that different systems use different data formats and standards. As mentioned earlier, hundreds of systems exist across the U.S. healthcare industry, and the lack of standardized APIs across EHR vendors is a serious problem.
According to recent data, only about 46 percent of U.S. hospitals had basic EHR interoperability. The rest are unable to easily share or extract data. Those EHR integration challenges and overall lack of interoperability aren't just inconvenient. It reportedly costs the healthcare industry billions of dollars annually. Pair that with data quality issues existing within these siloed systems, and integration becomes more than a simple bump in the road.
Privacy and Compliance Constraints in Healthcare Marketing
Another thing to consider when leveraging EHR workflow automation is data privacy. HIPAA tightly regulates the use of protected health information (PHI). Federal law limits what data practices can use for healthcare marketing automation. It also dictates how PHI must be stored, transmitted and secured. Therefore, practices wanting to establish EHR workflow automation and employ drip campaigns that use patient data must utilize HIPAA-compliant platforms. Otherwise, they face violating regulatory requirements.
EHRs are high-trust environments. They're purpose-built to protect sensitive information. Thus, practices must carefully navigate privacy rules or risk costly missteps.
Complicating matters, EHR vendors typically prioritize provider workflows over marketing integration. That means built-in marketing and outreach tools and capabilities are often limited or nonexistent.
Proven Workarounds for Healthcare Marketing Automation
While EHR integration challenges and regulatory concerns can make drip campaign automation seem impossible, practices use many effective workarounds to overcome these hurdles. One strategy is to use a phased integration approach. Transitioning to cloud-ready systems that support modern APIs makes it easier to share data with marketing automation tools later. Cloud-ready systems are more primed for seamless integration, communicating efficiently with other platforms while overcoming standardization and interoperability issues.
Another option is to use middleware or integration platforms that bridge EHR and healthcare marketing automation tools. They can translate across different formats and create more reliable drip campaign triggers without the need for extensive custom development.
Some practices also employ semi-automated workflows. With this approach, data extraction triggers manual review. Staff can then review the data before deploying a campaign. While it adds a manual step into the process, it can ensure accuracy and compliance.
Leveraging APIs and Integration Platforms for Workflow Automation
Practices can also overcome challenges and implement automated drip campaigns in healthcare using APIs and integration platforms. Standards-based APIs enable secure and reliable data exchange between EHR and marketing automation platforms. REST APIs and subscription-based approaches facilitate real-time data exchange whenever patient records change.
There are also many integration platforms available to practices. These platforms connect EHRs to CRM and email automation tools, including HubSpot, Salesforce and HIPAA-compliant email platforms. Integration platforms can sync contact records, trigger campaign sequences based on EHR events and even automate patient list segmentation.
Using APIs and integration platforms makes EHR workflow automation possible, despite the many inherent challenges. They reduce manual effort and maintain patient engagement through data-driven campaigns tailored to each patient.
Starting Small with High-Impact Campaign Triggers
EHR-driven patient communication automation isn't easy. Try starting small. Beginning with simple campaigns focused on appointment reminders, post-visit follow-ups or annual checkup messaging is a great way to start your practice's journey with this automation. You can utilize basic demographic information and appointment data to get into the swing of things before tackling more complicated clinical triggers.
It's an excellent opportunity to test the waters and roll out EHR workflow automation with more precision. Rather than going all in and making serious missteps, you can start slow and do things right. Furthermore, starting small helps you prove ROI and gain more support for advanced automation.
As your practice sees success with automation, make continuous improvements. Use those small campaigns to solve integration challenges and gradually expand your automated workflows. Work incrementally to scale automation safely.
Build Patient Engagement That Runs on Autopilot
Despite the seemingly insurmountable EHR integration challenges that stand in the way of patient engagement automation, success is achievable. Overcoming those hurdles can help your practice unlock consistent patient challenges without the manual work. Start small, address challenges and scale safely. Doing so can pave the way to reduced administrative burden, improved patient outcomes and greater success for your practice. Create the personalized experiences that patients deserve and unlock stronger revenue.
Automating Drip Campaigns from EHR Data: Common Roadblocks and Proven Workarounds
In healthcare, achieving and maintaining high patient retention rates is key to success. One study found that boosting retention rates by just 5 percent can increase profits by as much as 95 percent, all while improving patient outcomes and providing more operational stability.
General medical and dental practices have an average patient attrition rate of around 17 percent. However, that figure is typically much higher for specialty practices. Many specialty practices struggle to retain patients long-term, largely because they communicate with every patient the same way. Most practices provide generic outreach that feels impersonal and irrelevant to each patient's individual needs. That leads to missed opportunities to engage patients on a more personal level, ultimately impacting continuity of care and long-term revenue potential.
Fortunately, there is a solution. CRM segmentation allows specialty practices to deliver a more personalized experience for different patient groups. It's an opportunity to develop and apply patient retention strategies based on demographics, medical histories, treatment plans and more, keeping patients across your practice more engaged and eager to schedule return visits.
What Is Patient Segmentation in Healthcare CRM
Healthcare CRM patient segmentation is the process of dividing patients into distinct groups based on shared characteristics. Customer relationship management (CRM) software can create these groups using factors like:
• Demographics: Age, gender, income, location, etc.
• Treatment History: Past procedures or visit frequency
• Health Behaviors: Follow-up engagement or treatment adherence
• Clinical Needs: Post-treatment care, chronic condition management, etc.
In healthcare, segmentation helps practices tailor communication and care approaches to better match each segment's unique needs. Rather than using the same patient retention strategies and outreach tactics for every patient, your practice provides more relevant communications to keep each segment engaged. For example, practices can use segmentation to offer age-based wellness programs for specific age groups or to deliver condition-specific communication, education and reminders for patients managing the same ongoing concerns.
There are many ways to use segmentation. Not only does segmentation help improve patient retention in healthcare, but it also benefits the people your practice serves.
Why Specialty Practices Need Targeted Patient Retention Strategies
Specialty practices like orthodontics, dermatology, cardiology and more face significant retention challenges. General care practices benefit from routine check-ups that naturally keep patients engaged. That's an advantage that specialty practices just don't have. In most cases, patients come in for a specific treatment. Once your practice helps resolve their health concerns through treatment, patients don't come back.
As a result, it's tougher for specialty practices to build those long-term patient relationships. Continuity of care, including follow-up visits, ongoing screenings and condition management, depends entirely on patients staying engaged beyond a single visit. Practices must build those relationships, and generic outreach just won't cut it.
Personalized outreach is key, and it works. One survey found that 62 percent of healthcare professionals believe that personal communication is critical. Another study unveiled that up to 91 percent of patients are more likely to stick with a healthcare provider that offers more tailored experiences, and personalized outreach can boost overall patient engagement by as much as 20 percent.
Common Patient Segmentation Types for Better Engagement
There are many ways to approach specialty practice patient segmentation. Practices can create several types of patient groups, each of which can pave the way for more personalized communication and care.
Demographic segmentation groups patients by characteristics like age, gender, income or location. Group demographics make it easier to fine-tune patient retention strategies based on patient needs. For example, practices can tailor outreach by providing age-appropriate education, offering preventive care reminders, providing information about relevant screening needs or delivering financial messaging that aligns with patient circumstances.
Behavioral segmentation is another common factor that can separate patients. These groups focus on how patients interact with the practice. Practices can use CRM segmentation to create groups based on treatment adherence, appointment history, missed visits or engagement with previous communication. Behavioral data can identify those patients who may require appointment reminders, additional education or proactive outreach.
Clinical segmentation dives into patient needs. Practices can create segments based on diagnosis, risk levels, treatment plans and more. Clinical CRM segmentation creates the opportunity for condition-specific outreach, follow-up scheduling and ongoing care management, ensuring that all communication correctly matches a patient's clinical needs.
Building Segments That Drive Patient Loyalty Programs
Effective healthcare CRM patient segmentation goes beyond single data points. While looking at simple demographics and clinical data is easy, personalizing communications at scale requires precision. The best approach is to create actionable segments by combining multiple criteria to paint a more complete picture of each group. It's about taking several data points to fully understand which type of outreach will resonate most with each segment.
For example, practices can create groups that include high-value patients with chronic conditions who may need regular monitoring. Communications with that group will differ significantly from those with low-value patients, who may only be interested in ongoing health screenings.
The trick is to use CRM data to identify patterns across demographics, health histories, clinical data and behavioral data. The goal is to study all data available to create actionable insights that matter.
It's important to remember that this data isn't static. It evolves as patients navigate their healthcare journey and build lasting relationships with your practice. Therefore, segments require regular updating. Updates ensure that loyalty programs, outreach efforts and patient retention strategies reflect current patient circumstances rather than outdated assumptions.
Targeted Patient Outreach Tactics for Each Segment
Every segment is different, requiring separate communication strategies to stay engaged. When your outreach reflects a patient's distinct needs, risk levels and mindset, the more likely it is that communication will resonate. Let's look at a few examples.
High-risk patients typically benefit from more frequent check-ins and reminders. Structured communications make a difference. Your outreach can include appointment reminders, follow-ups after a visit, medication reminders and clear next-step guidance. Consistent communication can reinforce care plans while helping patients feel supported.
Patients focusing on wellness often respond best to educational messaging and preventative information. Outreach for this segment might incorporate routine screening reminders, invitations to patient loyalty programs or educational content that supports their long-term wellness goals. This type of communication shows the value of ongoing engagement, even when there's no immediate need for treatment.
Finally, there are the disengaged patients or treatment avoiders. This group requires a more cautious approach, as high-pressure outreach can often deter them from visiting your practice. Communications to this segment might include low-pressure educational content, messaging about the importance of follow-up care and information about common concerns.
Automating Segmented Communication for Consistent Engagement
Automation makes segmentation and specialty practice patient engagement work at scale and with impressive precision. With automation, your practice can deliver the right messaging at the right time without overburdening staff. It's what makes modern patient retention strategies successful, allowing you to keep communications relevant while ensuring that no patient falls through the cracks.
There are many ways to use automation to your advantage. For example, you could send automated appointment reminders timed to patients' preferences, send post-treatment follow-ups that automatically trigger when patients reach specific care milestones or deliver educational content tailored to conditions.
The best part is that automation saves your practice time. Handling outreach manually is both time- and labor-intensive. Automation can reduce administrative workload by 30 percent, saving hundreds of hours of manual work and allowing teams to focus on higher-value patient interactions.
H3: Measuring Success of Your Segmentation Strategy
Like anything else, practices must track the success of patient retention strategies and segmentation. Here are a few metrics your practice should track across groups:
• Appointment Show Rates: Tracking show rates can unveil which tactics keep specific groups engaged.
• Patient Lifetime Value: This metric highlights high-value segments to guide resource allocation.
• Treatment Acceptance Rates: Treatment acceptance rates can provide insight into how different segments respond to care recommendations.
• Return Visit Frequency: Return visit data can indicate whether or not groups stay engaged over the long term.
These metrics and more can highlight which tactics work and which don't. There's no magic formula to targeted patient outreach. Following these data points allows practices like yours to refine your approach based on real results. Use these metrics to adjust messaging, outreach frequency and delivery channels as you optimize your tactics.
Start Building Patient Relationships That Last
Successful healthcare CRM patient segmentation turns your approach to optimizing patient retention from reactive to proactive. When done right, segmentation can lay the groundwork for improved patient outcomes, greater satisfaction, higher retention rates and stronger practice revenue. Even simple segmentation, when applied consistently, creates a more personalized journey for patients while making your patient retention strategies measurable. Patients stay engaged, return for follow-ups and stick around to build a lasting relationship with your practice.
With Fuse, you can take the first steps toward patient segmentation during the intake and insurance verification process. Schedule your demo today to learn more.
How CRM Segmentation Improves Patient Retention for Specialty Practices
Healthcare pricing transparency is no longer optional. As of 2022, it's now federal law. The No Surprises Act and new hospital price transparency rules have reshaped how providers, practices and hospitals all share pricing information. Healthcare professionals are now legally obligated to provide patients with realistic cost estimates before rendering care.
With recent surveys showing that over 90 percent of Americans are in favor of that transparency, these regulations align with what patients want. It's up to providers to comply. Failing to do so could result in civil penalties, billing disputes, legal issues and patient dissatisfaction.
In this guide, we'll cover what's required and how providers can stay compliant, ensuring your practices meet the mark while also supporting patient expectations.
Understanding the No Surprises Act and Good Faith Estimates
The No Surprises Act (NSA) is a law designed to protect patients from unexpected medical bills. As the name implies, it helps prevent surprises while promoting greater patient cost transparency, especially concerning out-of-network or ancillary providers that patients typically do not choose. The federal law went into effect in 2022, now requiring healthcare organizations to clearly communicate potential charges before providing service, empowering patients to make informed financial and care decisions.
The NSA is complex and comprehensive, but there are a few key components providers need to be aware of. One example is the Good Faith Estimate (GFE) requirement. A Good Faith Estimate is a written, itemized cost estimate detailing all the expected charges the patient will need to cover.
Who Must Provide Patient Cost Estimates?
- Under the No Surprises Act, all healthcare providers and facilities that schedule services for uninsured or self-pay patients must provide a Good Faith Estimate. This includes hospitals, physician practices, labs, imaging centers, ambulatory surgery centers and more.
- Keep in mind that Good Faith Estimates and general patient cost estimates are different. The former is required by law in certain instances. Meanwhile, general estimates for insured patients are generally not mandatory, as transparency obligations lie with health plans and insurers, not providers.
- The GFE requirement applies when providers and facilities schedule service at least three days in advance. The provider that receives the initial request for a GFE becomes the "convening provider or facility." Therefore, it's their responsibility to deliver a timely estimate. When multiple service providers and facilities are involved in a patient's care, it's the convening provider that must obtain cost data from all parties involved and include it on a single GFE.
- There are exceptions for emergency care and unscheduled visits. Because emergency care happens so quickly, providers are exempt from GFE requirements.
- Now, the rules surrounding pricing transparency and Good Faith Estimates are federal law. The NSA is the baseline, but several states impose additional or slightly different requirements. For example, California, New York and Massachusetts all have distinct regulatory requirements that interact with, or sometimes overlap with or exceed, the NSA.
- Providers must check with their respective state legislature for any specific rules that augment those federal requirements.
Good Faith Estimate Requirements for Uninsured Patients
Good Faith Estimates are required for uninsured patients or patients who choose to self-pay. It doesn't matter if a patient has active insurance or not. If they decide not to use it, opting to pay out of pocket, they're within their right to request a GFE.
The NSA requires hospitals and providers to supply an accurate and easily understandable GFE at least one business day before a patient's scheduled appointment. It must include all reasonably expected charges. That includes everything, not just provider fees. It must detail costs associated with the facility, laboratory work, supplies, equipment and other relevant expenses.
For accessibility, GFEs must also be clear and understandable. These Good Faith estimate requirements ensure that documents don't contain complicated legal or financial jargon that the average patient wouldn't understand. GFEs are there to support patients, not confuse them.
Of course, accuracy is vital. If a patient's final bill is $400 or more above the original estimate, they have the right to file a payment dispute through the Patient-Provider Dispute Resolution process.
Cost Transparency Rules for Self-Pay Patients
As mentioned earlier, self-pay patients have the same rights as uninsured patients, regardless of whether they have active coverage. There are many reasons why someone might choose to pay out of pocket rather than use their insurance coverage. Some examples include high deductibles, privacy concerns or out-of-network care. Whatever the case, self-pay patients are entitled to a GFE.
Providers also can't assume insurance coverage. When a patient indicates they want to pay out of pocket and not utilize insurance, providers must offer a GFE.
Hospital Price Transparency Requirements
The Hospital Pricing Transparency rule is another piece of legislation that's changed the game for patients. It's similar to the NSA, aiming to help prevent surprises that could have significant financial implications for patients. This rule took effect in 2021 and requires all hospitals operating within the U.S. to publicly share their pricing.
Pricing must be available in two formats:
•Machine-Readable File: Machine-readable files are massive documents that contain comprehensive pricing data for all services and items the hospital might bill. These files allow technology developers, insurers and researchers to analyze pricing data at scale. Patients can also access these files to search for specific data points.
•Consumer-Friendly Display: These consumer-facing displays must highlight at least 300 "shoppable services." These include standard procedures or tests. As the name suggests, this format aims to be accessible to everyone. Usually, these displays are available on hospital websites.
Compliance and Enforcement of Healthcare Pricing Transparency
There's no way out of hospital price transparency. Failing to comply with this rule can result in serious legal and civil consequences. The Centers for Medicare & Medicaid Services is responsible for enforcing transparency rules.
Penalties can vary based on the size of the hospital. Facilities with fewer than 30 beds will receive a penalty of up to $300 per day of non-compliance. Meanwhile, larger hospitals may incur a penalty per bed, up to $5,500 per day. Annually, non-compliance penalties can reach millions of dollars!
Enforcement and subsequent penalties vary. States can impose additional rules and have stricter requirements that hospitals must follow. Hospitals can receive penalties at both the state and federal levels.
Furthermore, patient disputes and non-compliance lawsuits can add further financial burden. Failing to comply can cost your organization more than you might realize, and there is a real risk of experiencing penalties, even if you haven't yet.
Compliance isn't universal. Many hospitals have yet to fully comply with hospital price transparency rules. One study found that as of 2024, just over 21 percent of hospitals in the country are compliant.
Key Components of Compliant Patient Cost Estimates
To meet federal standards, patient cost estimates must include several key elements:
•Format: Patients must receive precise, readable estimates in a format that's easy to access, including printed paper or electronically delivered documents.
•Timing: Providers must deliver estimates at least 24 hours before a scheduled service.
•Comprehensiveness: Estimates must be comprehensive, detailing all relevant costs. This includes provider fees, facility fees, lab work, imaging, supplies, equipment and other related expenses.
•List of Providers: Estimates need to identify all providers associated with a patient's care, as well as fees paid to them.
•Service and Diagnosis Codes: When available, providers must record CPT codes related to a patient's care.
•Disclaimers: Every estimate needs a disclaimer that states the estimate isn't a final bill, and that the total may change based on unforeseen circumstances.
Accuracy is vital. Cost estimate regulations require that prices must reflect reasonable expectations. Providers can't lowball estimates to make services appear more affordable than they are.
Timing and Delivery of Good Faith Estimates
The timing of the estimate delivery matters, and what's required all depends on how far ahead a patient's service is scheduled.
For appointments scheduled three days or more in advance, providers must supply a GFE at least one business day before their visit. Services scheduled less than three days in advance require delivery of the GFE at the time of, or just before, the service.
Any patient who requests an estimate must receive it within three business days, regardless of whether they're uninsured, self-pay or fully insured.
As mentioned earlier, providers can supply a physical copy of the estimate, delivering it in person. Alternatively, patients can receive it electronically. Either way, patients must acknowledge receipt of the estimate.
Common Challenges Healthcare Providers Face with Cost Estimate Regulations
Providing Good Faith Estimates and pricing transparency is legally required, but that doesn't mean it's easy. There are many challenges involved. Practices must face changing contracted rates from payers, difficulties in chasing down data from multiple providers involved in a single patient's care, and uncertain patient needs.
Healthcare can change rapidly, and it's sometimes difficult to forecast what tests or procedures a patient will need.
Additionally, GFEs and price estimates can place an administrative burden on healthcare providers and their staff. Technical limitations often make creating accurate estimates a time-consuming and labor-intensive process.
Unfortunately, these are all challenges that providers have no choice but to navigate. Accurate estimates and complete transparency are now legally required, and patients want it. Failing to comply could result in penalties and eroded patient trust.
Streamline Cost Estimate Compliance with Automation
Fortunately, there are ways to get around those challenges. Automation is helping hospitals and providers create Good Faith Estimates quickly and easily, all without the worry of human error. Automated systems like Fuse can pull real-time data to calculate patient responsibilities in seconds.
With Fuse, you can reduce staff workloads, improve accuracy and make your practice audit-ready. Fuse can transform your organization for the better, help you earn your patients' trust, and ensure compliance with all applicable laws.
Schedule your Fuse demo today to learn more and discover how easy it is to create price cost estimates that your patients will appreciate.
Patient Cost Estimate Regulations: What Healthcare Providers Need to Know
Price for Behavioral Health Care with Anthem
For healthcare providers, one of the most persistent challenges is determining if they are being paid a fair rate. Understanding how your reimbursements compare to the rest of the market is essential for contract negotiations and financial planning.
The CMS Price Transparency mandate now allows providers to look directly at the negotiated rates between payers and facilities. By accessing these machine-readable files, we can analyze the "allowed amounts"—the maximum amount a plan will pay for a covered health care service.
Benchmarking Anthem Blue Cross California Rates
To provide a clear picture of the current landscape, we filtered the latest transparency data for Anthem Blue Cross California specifically for Behavioral Health CPT codes.
Below are the negotiated rate results for key CPT codes:
- CPT 90791 (Psychiatric Diagnostic Evaluation)
- Unique NPI Count: 20,492
- Mean Negotiated Rate: $186.81
- Median Negotiated Rate: $142.25
- CPT 90837 (Psychotherapy, 60 minutes)
- Unique NPI Count: 20,493
- Mean Negotiated Rate: $159.79
- Median Negotiated Rate: $121.72
- CPT 96130 (Psychological Testing Evaluation, 1st hour)
- Unique NPI Count: 5,567
- Mean Negotiated Rate: $273.58
- Median Negotiated Rate: $224.60
Key Insights from the Data
The data reveals the following benchmarks for Anthem's behavioral health network in California:
- 90791 (Diagnostic Evaluation): The median rate for an initial evaluation sits at $142.25. The significantly higher mean of $186.81 indicates that a portion of the 20,000+ providers in this network have negotiated rates well above the midpoint.
- 90837 (60-Minute Psychotherapy): As one of the most frequently billed codes, the median negotiated rate is $121.72.
- 96130 (Testing Evaluation): This specialized service commands the highest reimbursement in this set, with a median rate of $224.60.
Disclaimer: The data provided is based on publicly available CMS machine-readable files and represents a snapshot of negotiated rates. Individual reimbursements may vary based on provider credentials, specific contract terms, and facility type.
What is the Average Allowed Amount for Behavioral Health in California with Anthem Blue Cross?
According to census data, over 90 percent of people in the United States have some form of health insurance. For hospitals and practices, a vast majority of annual revenue comes from payer reimbursements. However, an uptick in claims denials is creating a massive source of revenue loss and administrative burden for providers.
The biggest driver for denied claims? Inefficient and inaccurate insurance verification processes.
Proper insurance verification is vital for providers and organizations. In simple terms, insurance eligibility verification is the process of confirming a patient's coverage before rendering any services. It involves verifying that policies are active, understanding what services are covered, determining a patient's financial responsibilities and more.
Today, insurance eligibility verification is more crucial than ever. Increasing out-of-pocket costs, changing policies and increasingly complex plans are creating new challenges for both patients and providers. Practices that fail to verify patient insurance details upfront expose themselves to frequently denied claims and severe cashflow issues.
Understanding the Insurance Eligibility Verification Process
Patient insurance verification is a front-end check that involves confirming coverage before providing service. When done correctly, it can prevent patients from receiving unexpected bills while mitigating the risk of denied claims for providers. The process sounds simple, but it's more complex than most realize. Here's a quick breakdown of how medical insurance verification works.
• Patient Information Collection: During the intake process, practices need to collect accurate patient information, including their name, date of birth, policy numbers and more.
• Checking Coverage Status: Next, the staff needs to confirm that policies are active on the date of service. They must also check that the practice is within the payer's network.
• Verifying Benefits: At this point, practices must discover what's covered and what's not. They also need to be aware of any limits or excluded services.
• Identifying Patient Responsibilities: During this process, practices must also verify details like co-insurance, copays and deductibles.
• Understanding Prior Authorization Requirements: Some CPT codes require additional documentation and a more detailed approval process before payers will cover services. Practices need to understand these requirements to prevent outright claim denials.
There are several methods for performing medical insurance verification, including using payer portals. However, portals often aren't enough to understand the nuances of patient eligibility. Some details, such as prior authorization requirements, require staff to call payers directly. Calls are often the only way to understand the requirements of CPT code-level benefits, but they come at the cost of time and administrative resources.
Key Steps in the Process
Now that you understand what the process entails, let's examine the actual workflow for verifying a patient's insurance coverage.
• Collect Patient Demographics and Insurance Details: Start by gathering relevant patient data. You'll need their full name, date of birth, policy number, group number and plan name. If covered under a shared plan, you'll also need to record the relationship with the insured. Accuracy is crucial here, as even simple errors can lead to delays and claim denials.
• Submit Data to Payers: The next step is to submit the collected information to payers, either through their online portal or through the phone. Make sure to note the method used to submit information and record any reference numbers provided.
• Review Responses: After payers respond, you'll need to review coverage dates, in-network status, benefits details and all other relevant data.
• Document Patient Responsibilities: Payers also respond with information about copays, deductibles and co-insurance. Record all out-of-pocket costs that patients will need to pay, and communicate with the patient early on.
• Obtain Prior Authorizations (If Necessary): If any CPT codes require prior authorization, you must initiate that process as soon as possible to prevent delays. Depending on the payer, you may need to submit documentation such as clinical notes, patient medical history and lab results.
Collecting Accurate Patient Information
Inaccurate information leads to instant denials, negatively affects revenue cycle management and creates tons of extra work for your staff. Your team needs to gather complete and accurate information upfront. That means requesting to see both sides of an insurance card, double-checking all policy numbers and confirming the spelling of all names.
If working with existing payments, don't assume that nothing has changed. Always review the information you already have and verify it for accuracy.
To reduce errors during the data collection phase, follow these tips:
• Check name spellings and policy numbers multiple times
• Scan or photograph cards for record-keeping and reference
• Use standardized forms and checklists to ensure staff gather all pertinent data
Methods to Verify Patient Insurance Coverage
As mentioned earlier, there are several ways to verify a patient's insurance coverage.
• Phone Calls: The old-school approach still works. Staff can call payers directly to confirm coverage and benefits. While it is thorough, this method is time- and labor-intensive. Plus, it's still prone to human error.
• Payer Portals: Online payer portals simplify things, allowing practices to check coverage without speaking on the phone. Online portals can be faster to use, but they're often incomplete. That's especially true when learning about prior authorization requirements.
• Automated Verification Software: Automated verification software is quickly becoming the new standard, and it's not hard to see why. Software platforms integrate with existing EHR and practice management platforms, pulling live payer data to verify insurance eligibility in seconds. They can even perform real-time insurance verification checks, significantly reducing administrative work while virtually eliminating the risk of human error.
How Verifying Insurance Reduces Claim Denials
Verifying insurance upfront allows your team to catch potential issues before submitting claims. Whether you're dealing with missing authorizations, inactive policies, or are about to serve a patient with an out-of-network policy, thorough verification processes ensure you catch those issues early. As a result, you save time and experience fewer denied claims.
Claims denials aren't just frustrating. They're also costly. In 2023, the healthcare industry reportedly spent $18 billion overturning denied claims. Reworking a single denied claim can cost your practice anywhere from $25 to $118. Furthermore, delayed reimbursements caused by denials and reworks can impact your cash flow for over four months. Pair all that with hours of additional administrative work addressing issues that resulted in the denial, and you're looking at substantial financial implications.
Denials can render effective revenue cycle management impossible, hindering your practice's growth while also contributing to a negative patient experience.
The Role of Prior Authorization in Medical Insurance Verification
Prior authorizations add some confusion and complexity to insurance verification processes. Certain services, such as high-cost procedures, hospital admissions, imaging tests (including CT scans and MRIs) and medical equipment, among other things, require additional documentation before payers will cover them.
Ignoring prior authorizations, whether intentionally or unintentionally, can lead to issues such as instant denials, payment delays and surprise bills for your patients. Furthermore, your practice will need to spend time and resources on costly reworks or appeals.
Insurance verification can help you avoid all that. When performing eligibility checks, your team must always review prior authorization requirements and initiate the relevant processes before proceeding with claims submission.
Benefits of Automated Patient Insurance Verification
Manual insurance eligibility verification is certainly adequate, but it's not the most efficient way of doing things. Manual processes are prone to human error. It's also laborious, taking substantial time to complete while wasting valuable staff resources.
Automated patient insurance verification addresses those pain points and more. Technology streamlines the process from start to finish, with automation performing eligibility checks in real time, eliminating concerns about wasted resources or human error. Additionally, automated systems are scalable and grow with your practice.
That's not all.
Automated systems also enhance the patient experience. Not only does the improved accuracy prevent surprise bills, but it can also facilitate faster check-ins. Real-time patient eligibility verification confirms coverage in seconds, all without the need for mountains of paperwork or lengthy wait times.
Your staff benefits, too. Because software handles the heavy lifting, there's no need to talk on the phone, perform manual patient checks or rework claims due to mistakes. Automated patient verification even lowers the risk of denials and billing errors.
Ultimately, automated systems are the ultimate solution for fast, accurate and comprehensive insurance verification. Software will help your practice work more efficiently, enhancing revenue cycle management while maintaining a strong cash flow.
Improve Your Revenue Cycle with Streamlined Verification
With numerous changes affecting the insurance industry, inadequate verification processes can significantly impact your practice. Improving your approach makes all the difference. Strong insurance eligibility verification is the foundation of a healthy revenue cycle. Confirming coverage upfront can lead to fewer denials, leading to faster reimbursements and more predictable cash flow.
Let Fuse help transform the way your practice handles insurance verification. Fuse is a solution that automates verification processes to improve accuracy, reduce administrative burden and optimize efficiency. With Fuse, you can spend less time dealing with delays and claim reworks. Instead, you'll enjoy more time with patients, predictable revenue and happier staff.
To see how Fuse can revolutionize your verification workflow, schedule your demo today.
Why Verifying Insurance Is Critical for Healthcare Providers
Since the No Surprises Act took effect in 2022, healthcare price transparency has become a top priority for hospitals, providers and patients. This act transformed many aspects of medical billing, aiming to protect patients from surprise bills while also providing them with crucial information to make informed decisions about their care.
The law is comprehensive, but pricing transparency is one critical aspect that practices and healthcare organizations must comply with. Accurate price estimates not only meet transparency requirements, but they are also something that patients expect. Poor patient cost estimate accuracy falls short, and that could impact patient trust, satisfaction and even payment likelihood.
Even still, many organizations struggle to supply accurate patient fee estimates. In 2023, one report found that just 36 percent of hospitals complied with price transparency rules. As of 2024, the Centers for Medicare & Medicaid Services (CMS) had received over 16,000 complaints regarding potential violations. Recent data also suggests that arbitration related to the No Surprises Act is increasing healthcare spending waste, affecting practices like yours.
Accurate patient fee estimates are more crucial than ever. In this guide, you'll learn five proven solutions to help your practice improve estimation accuracy, fulfilling your legal obligations under the No Surprises Act while also meeting patient expectations.
Leverage Advanced Healthcare Price Transparency Tools
Pricing transparency begins with feature-rich patient payment estimation tools. Leveraging technology can help your practice fulfill transparency requirements without the administrative overhead. Manual processes often require hours of dedicated work, which software can do faster and more accurately.
The best tools integrate with EHR and practice management systems, pulling relevant data from payer contracts and portals to accurately calculate potential out-of-pocket costs. Features like granular insurance verification provide up-to-date information and verify coverage at the CPT code level. By pulling data from procedure cost databases, patient payment estimation tools can deliver more precise figures, leaving little room for guesswork or error.
More advanced tools can even estimate copays and perform automated deductible calculations after confirming benefits. Modern solutions can utilize granular benefits data from payers to improve medical billing accuracy and create more precise estimates for patients.
Implement Comprehensive Patient Cost Estimation Workflows
Structured and comprehensive workflows ensure that accuracy isn't left to chance, but instead becomes a repeatable operational capability for your practice. Start by establishing an estimation process. A solid workflow can look like this:
1. Appointment Scheduling
2. Patient Onboarding
3. Insurance Verification and Benefits Checks
4. Estimate Generation and Delivery
Patient payment estimation tools will do much of the heavy lifting, but staff should stick to a well-defined workflow to ensure that every estimate is accurate and delivered accordingly. Train your team to follow the workflow and utilize the tools your practice employs to their full advantage. Staff should be knowledgeable about interpreting eligibility responses and following benefits checking protocols.
Insurance benefits verification should occur 48 to 72 hours before a patient's scheduled visit. Those eligibility checks should trigger the automatic generation of a patient fee estimate, allowing your practice to deliver the information within 24 hours. The sooner patients receive pricing information, the better.
Enhance Data Quality for Better Patient Fee Estimation
High patient cost estimation accuracy hinges on the quality of your data. Unfortunately, inconsistent and outdated data is a significant source of discrepancy between what estimates practices provide and what patients actually end up paying. Common issues that providers face when creating estimates include:
• Imprecise CPT Codes
• Missing or Inaccurate Code Modifiers
• Failing to Separate Professional and Facility Fees
Not using code modifiers is a particularly frustrating issue. Modifiers help to provide more information about a service or procedure. Failing to use them or doing so incorrectly can significantly impact medical billing accuracy. Yet, it's surprisingly common, with one study finding that up to 59 percent of code modifiers used in encounter data didn't match clinical data.
To prevent data quality issues, regular audits and routine data cleanup processes are essential. Strong data governance ensures that downstream processes, such as patient fee estimation, don't rely on outdated or incorrect information.
Establishing Good Faith Estimate Healthcare Standards
Under the No Surprises Act, providers must supply Good Faith Estimates (GFEs) to uninsured and self-pay patients when requested.
Best practices recommend that all patients become informed of their right to a GFE. When scheduling patients, staff should notify uninsured and self-pay patients of GFE availability. Practices also need to familiarize themselves with compliance requirements, create replicable templates and ensure GFEs are in clear, understandable and accessible formats.
It's also important for practices to keep versioned documentation for every estimate. Separate versions can help keep track of estimations when the scope of care changes. If that happens, practices must have a clear protocol for delivering an updated estimate and communicating changes to patients. Under the law, practices must supply an updated GFE when scope changes result in changes to expected charges.
The No Surprises Act also includes strict documentation standards. Every GFE requires the following information:
• Patient Name
• Date of Birth
• Description of Services Provided
• Itemized List of Costs
• Diagnostic and Service Codes Associated with Each Service
• Provider Name, NPI and Tax ID Number
• Practice Address
Improving Medical Billing Accuracy Through Training
Powerful patient payment estimation tools go a long way, but that doesn't mean your staff doesn't need training. Software can handle much of the complexity involved, but your team needs to understand insurance plan verification, common coding errors, payer contract nuances, modifier usage and accuracy issues.
Invest in staff education. Ongoing training programs can ensure your team is well-equipped to handle any challenge that arises while actively working to improve estimation accuracy. Help your staff update their certifications and implement strict quality assurance measures.
Empowering your team through training and education makes a significant difference, enabling them to deliver more accurate estimates, communicate more effectively with patients and help prevent discrepancies that cause unwanted billing surprises.
Selecting Patient Payment Estimation Tools That Scale
Choosing the right tools is just as crucial as creating efficient workflows and addressing data quality issues. Tools can make or break your practice's approach to delivering patient fee estimations, ultimately impacting your ability to comply with the law and meet patient expectations.
Review your options and choose a software platform that can scale with your practice. As your needs evolve, you must have tools that can adapt and grow with you. Consider integration capabilities, reporting features and the quality of vendor support. The best options will integrate seamlessly with your existing EHR and practice management systems, all while offering comprehensive reporting capabilities. You also want to ensure that software vendors provide robust support that'll keep operations running smoothly, no matter what challenges you encounter.
Also consider how software can impact your bottom line. Will it speed up insurance verification and estimate generation? How much admin time can a platform save your practice, and how accurate is the software's approach to calculating estimates? The answers to those questions matter.
Maximize Patient Satisfaction with Transparent Cost Estimates
Accurate patient fee estimates make all the difference, improving both patient satisfaction and collection outcomes. One study found that upfront pricing transparency can lead to a 27 percent increase in upfront patient payments. Meanwhile, patient satisfaction increases by up to 88 percent.
The truth is that patients want and expect healthcare price transparency through accurate estimations. With new laws requiring providers to be more upfront about patient costs, taking steps to deliver more precise estimates could benefit your practice in more ways than one.
Let Fuse build trust with your patients and reduce surprise bills. Fuse is an end-to-end solution for CPT code-level insurance verification and patient fee estimates. Fuse calculates exact out-of-pocket costs for every visit, supporting your quest for complete transparency while also improving your practice's revenue cycle.
Request your Fuse demo today to see how it works in the real world and discover how improved patient cost estimation accuracy can benefit your practice.
How to Improve Patient Fee Estimation Accuracy: 5 Proven Strategies
Healthcare costs are at an all-time high. In 2023 alone, healthcare spending in the United States reached $4.9 trillion. With the cost of care and insurance continually increasing, patients are more anxious about visiting healthcare providers than ever.
One study found that over a third of Americans have skipped or postponed healthcare due to worries about the costs. Over half of surveyed adults said it's difficult to afford healthcare, and 62 percent said they were worried about their ability to afford it in the future. About 45 percent fear that a significant health event will bankrupt them.
Those numbers are staggering, and surprise bills only exacerbate those worries. These days, patients require medical billing transparency and failing to provide it could erode the all-important patient-provider relationship by dampening trust. Fortunately, practices like yours can take steps to alleviate those worries by providing patient fee estimates.
The Power of Healthcare Cost Transparency in Patient Care
Having healthcare cost transparency isn't just nice to have in today's market. It's what patients want and expect. Centers for Medicare & Medicaid Services (CMS) regulations require hospitals to publish clear pricing information online, in both machine-readable and consumer-friendly formats. Failing to comply could result in substantial daily penalties and legal consequences.
The consumer-friendly version is particularly vital. One survey suggests that 92 percent of Americans support hospital price transparency, and a growing number of patients are shopping around for healthcare services. Compliance with CMS regulations and publishing consumer-friendly pricing information helps build confidence.
It establishes trust between patients and providers from the jump and empowers patients to make informed decisions about their care. It can reduce anxiety about healthcare costs and allow patients to get the care they need with confidence.
Patient Fee Estimates: Essential Tools for Modern Healthcare
Patient trust in healthcare is crucial, and the best way to earn it is by being transparent and open. Effective patient fee estimates are more than just simple totals printed on a piece of paper. They're comprehensive, detailing the costs associated with a patient's care. They should also provide enough information about the services rendered to allow patients to make informed decisions.
The best patient payment estimator tools will provide specific categories detailing costs about:
• Individual Procedures
• Hospital Fees
• Facility charges
• Secondary Services
• Imaging
• Diagnostics
• Lab Services
• Preventive Care
• Aftercare
Estimates need to include all costs associated with the services rendered. For example, a patient coming in for a knee MRI might include estimate categories covering imaging fees, radiologist fees and lab costs.
For uninsured or self-pay patients, medical cost estimates are straightforward.
However, insured patients expect to see their financial responsibilities reflected against their insurance coverage. Therefore, estimates must account for these coverage nuances, including information about copays, co-insurance, deductibles and out-of-pocket maximums, among others. Comprehensive price breakdowns help to improve accuracy, eliminating the risk of surprise expenses.
Medical Billing Transparency: Reducing Patient Anxiety and Complaints
As mentioned earlier, patients want medical billing transparency. Roughly 9 out of 10 Americans are in favor of it. It's not hard to see why. Having a better idea of how much services will cost upfront makes it easier for patients to plan accordingly and make crucial decisions.
Healthcare cost transparency can significantly reduce anxiety while also boosting satisfaction. In one survey, 64 percent of patients reported that receiving accurate medical cost estimates and greater transparency increased their satisfaction with healthcare providers. That is something that can directly benefit your practice.
That's not all. Because patients know the costs upfront, they are also more likely to pay. In one study, practices that implemented advanced medical cost estimates and healthcare pricing tools saw a 27 percent increase in upfront payments. That information may even help improve your practice's collection rates.
Good Faith Estimates: Meeting Regulatory Requirements
The No Surprises Act, which took effect in 2022, requires hospitals and providers to provide Good Faith estimates to all self-pay or uninsured patients. There are several key compliance requirements when providing Good Faith Estimates, as mandated by law.
•Notice and Inquiry: When a patient schedules a service, providers must ask if they're uninsured or self-paying, informing them of their right to Good Faith Estimates.
•Timing: If scheduling services three days or more in advance, providers must offer the Good Faith Estimate within one business day. If scheduled 10 days or more ahead, providers have three business days.
•Content and Format: The estimate must include the patient ID, a description of each service and expected codes and charges. It also requires information about the provider and facility, as well as a disclaimer stating that estimates are subject to change.
Failure to comply with the No Surprises Act regulations could trigger civil penalties of up to $10,000 per violation, excluding any state-level sanctions.
Medical Cost Estimates for Insured Patients
Providing patient fee estimates to those with insurance can be challenging. Healthcare coverage contains many nuances, particularly from the patient payment perspective. The No Surprises Act also required that hospitals and providers offer an Advanced Explanation of Benefits (EOB) analysis.
This document outlines a patient's out-of-pocket costs, which may vary depending on their insurance coverage. Because deductible and co-insurance figures can change, providing accurate information isn't easy. Patients with multiple forms of coverage present even greater challenges.
Practices must coordinate with insurers to deliver accurate information. Failure to do so can result in billing disputes, patient dissatisfaction and delayed payments. A strong relationship with insurers and real-time eligibility tools can help practices overcome those challenges, protect their revenue cycle and maintain patient satisfaction.
Transform Patient Experience with Accurate Healthcare Pricing Tools
Providing accurate patient fee estimates while maintaining medical billing transparency doesn't have to be difficult. Fuse is a platform that benefits practices of all sizes, leveraging automation to simplify how you provide estimates. In addition to streamlining patient intake and insurance verification, Fuse creates estimates that can help increase patient satisfaction, decrease billing inquiries and improve collections. Fuse utilizes granular benefits data from payers, ensuring accuracy regardless of the complexity of a patient's insurance coverage.
With strong integration capabilities that work with your existing systems and workflows, Fuse can take your practice to the next level while enhancing your current operations. Reach out today to schedule your Fuse demo and see how much of a difference patient fee estimates can make.
How Patient Fee Estimates Build Trust and Transform Healthcare Relationships
In this video, I walk you through how to conduct your first phone call for insurance checks. I explain the importance of setting up your check settings and creating a template that allows for both portal and phone call checks. You'll learn how to add a new patient and select the appropriate template to get the most accurate results.
How to Run Your First Insurance Check Phone Call
Despite increasingly powerful automation capabilities, many healthcare practices still rely on outdated manual processes for insurance eligibility verification. If your practice is one of them, you're likely bleeding revenue without realizing it.
Insurance verification costs for the medical industry amount to $42 billion annually, with 98 percent of that figure spent by healthcare providers and organizations. It may come as a surprise, but a significant portion of the annual spend on insurance verification in healthcare comes down to errors. In one survey, approximately 56 percent of respondents said that denied insurance claims resulted from mistakes during the intake and insurance verification processes.
With every mistake comes hours of work, increased administrative burden and tons of hidden costs. In the end, practices spend up to $118 reworking denied claims. Needless to say, that figure adds up and seriously impacts healthcare revenue cycle management.
In this guide, you'll learn about how healthcare billing errors and a poorly optimized insurance verification process can harm your practice's bottom line, and discover ways to change that.
How Healthcare Revenue Cycle Management Suffers From Eligibility Errors
When eligibility checks fail, the ripple effect is substantial. Mistakes often lead to initial claims being denied, resulting in severe frustration for patients. In addition to potential service delays, patients may encounter unexpected bills and additional costs. That all erodes trust and creates an awful experience for patients.
From a practice's standpoint, poor eligibility checks create hours of additional work. Staff must spend time identifying and correcting errors, as well as reworking claims. Additionally, practices suffer from unpredictable cash flow. Mistakes can extend accounts/receivable timelines by weeks. Each denied claim isn't just a missed reimbursement; it's additional labor costs associated with correcting the problem.
Many mistakes can occur during insurance verification. On the simpler side, human error during data entry is reportedly the cause for 60 percent of first-submission rejections. Meanwhile, missing prior authorizations account for 11.6 percent of denials. Service coverage problems account for over 10 percent, while eligibility problems make up over 26 percent.
The True Financial Impact of Coverage Check Problems
Poor insurance verification costs practices more than most realize. As mentioned earlier, reworking a single denied claim can cost anywhere from $25 to $118. Considering that denial rates sit at around 15 percent for hospitals and practices, that's a significant sum. Say that your practice has 500 denied claims in a single year and must spend $50 reworking them. That's $25,000 in administrative costs.
If that sounds far-fetched, consider this: In 2023 alone, providers spent over $25 billion contesting and reworking claims. For hospitals, denied claims cost about five percent of patient revenue. One study found that billing staff spent up to 60 percent of their time reworking denials rather than focusing on actual revenue-generating tasks. But that's not all.
The unnecessary costs incurred for insurance eligibility verification can hinder your practice's ability to grow. You spend more resources correcting mistakes, all while dealing with delayed reimbursements and cash flow that's far too unpredictable to make meaningful investments in the practice.
Common Insurance Verification Mistakes That Drain Practice Revenue
Several recurring errors can quietly drain your practice's revenue potential.
• Outdated Patient Information: Incorrect ID numbers, names or demographic information can trigger automatic denials. Practices like yours must confirm those details during every visit to prevent reworks and resubmissions.
• Missing Prior Authorizations: Failing to identify prior authorizations will result in complete denial or significant delays. Comprehensive insurance eligibility verification to the CPT code level will help prevent missed requirements.
• Incorrect Benefit Details: Missing data about copays, deductibles, coverage tiers and other relevant details can result in denied claims or underbilling. Practices should perform real-time checks before a patient's scheduled service to fully understand costs.
• Timing Issues: Late verification or failure to update coverage data increases the risk of denied claims. Your practice should verify coverage before each visit and update regularly to keep data current.
Patient Eligibility Check Process Failures
The insurance eligibility verification process can break down at many points.
Manual verification workflows often create delays. Staff must spend time calling payers, manually checking portals, managing paperwork and more. Those manual processes can take up to 20 minutes per patient, resulting in bottlenecks and delays.
Meanwhile, inadequately trained staff can misinterpret plan data or miss specific details, such as prior authorizations or secondary coverage. Poor training can harm practice efficiency and create countless issues that ultimately lead to denials.
Finally, a lack of real-time coverage tools can prevent teams from quickly confirming benefits, leading to costly mistakes.
Those are just a few potential points of failure for insurance eligibility. There are many ways to improve eligibility checks, but automated solutions are among the most effective in preventing these mistakes and others.
Coverage Timing Problems That Cost Practices Money
Timing matters for insurance verification in healthcare. Because policies can change frequently, poor timing can increase financial risks. Perform those checks too early, and coverage could change. Perform them too late, and you might render the services before realizing a patient's policy won't cover it. Revenue cycle optimization is all about running checks at the right time.
The optimal window is roughly 24 to 72 hours before a patient's visit. Real-time insurance verification software and automated tools can also help you ensure you're working with the most current data.
Transform Your Practice Revenue With Accurate Verification Solutions
Healthcare billing errors and poor insurance verification processes don't have to cost your practice. Fuse is the ultimate solution for fast, easy and accurate insurance eligibility verification. With Fuse, your practice can reduce verification time by 90 percent.
Fuse streamlines the process from start to finish, dramatically reducing the risk of errors while freeing up your staff's time to focus on patients. Protect your practice's bottom line and revenue potential while enhancing the patient experience.
Request your consultation and Fuse demo today and see how much improving your insurance verification processes can transform your practice.
The Hidden Costs of Inaccurate Insurance Verification in Healthcare Practices
Insurance verification errors are among the leading causes of denied claims, and they're costing both patients and healthcare organizations. Recent surveys suggest that more than half of healthcare revenue cycle leaders report an increase in claims denials, and roughly 68 percent attribute this to inaccurate or incomplete patient data during the intake and verification process. For larger organizations, those denials are costing $3 to $5 million in annual revenue, with practices spending at least $25 to rework a single denied claim.
As insurance plans become increasingly complex and payer rules evolve, the situation is only worsening. Yet, many practices still rely on outdated manual processes, and those workflows are failing healthcare providers. With many already facing slow operations, staff shortages and shrinking margins, clunky verification processes can snowball into substantial financial and operational problems.
Let's explore those insurance verification challenges further and dive into solutions that can streamline the process, leading to more accuracy, faster reimbursements and stronger cash flow for your practice.
The Most Common Patient Insurance Coverage Challenges
Manual verification is both labor- and time-intensive. The average medical practice spends nearly 13 minutes with manual benefits verification, if not longer. For a practice that handles 30 patients a day, that's over six hours of manual work. It's a significant staff resource drain, but that's not all.
With manual work comes the potential for human error and concerns about accuracy. Research indicates that error rates for manual workflows during medical coverage verification are roughly 27 percent. When those mistakes occur, staff need to spend even more time correcting them, effectively doubling or tripling the amount of time spent on a single patient's medical insurance verification.
As you can imagine, all that time and effort add up, creating bottlenecks that increase patient wait times and staff frustration. It's a vicious cycle with ripple effects that impact your team, your patients and your bottom line.
Why Insurance Verification Challenges Are Getting Worse
Insurance verification challenges are becoming a tougher mountain to climb for practices like yours. The growing complexity of modern healthcare isn't making things easier. Plans are more nuanced than ever before, and frequent policy changes are making it more difficult for administrators to keep up. Pair all that with narrow network tiers and the need for patients to have multiple forms of coverage, and it becomes increasingly difficult to streamline benefits verification while maintaining manual workflows.
It's not just practices and healthcare organizations that struggle to navigate today's insurance landscape. About 36 percent of insured adults struggle to understand what their own policies do and don't cover.
Those challenges continue to compound, complicating the process from the start. Furthermore, each layer of complexity increases the risk of error, leading to more denials, slower payments and more administrative costs. There are more puzzle pieces than ever, and old-school manual approaches no longer suffice.
Financial Impact of Poor Benefits Verification
The ideal insurance denial rate for hospitals and practices is 5-10%. Yet surveys show that actual denial rates are above 15 percent. Claims adjudication costs healthcare providers a staggering $25.7 billion annually, with an estimated $18 billion of that figure wasted due to reworks and re-submissions.
Administrative costs associated with denied claims exceed $57 per claim, with some hospitals incurring expenses of up to $181 to rework them.
Because medical coverage verification lies at the front of the process, failures during that crucial step cost practices downstream. Even the simplest mistakes can create benefits verification issues that tie up resources and drain cash flow. Every mistake during verification can result in greater delays for accounts receivable, increase administrative overhead and strangle overall practice efficiency.
How Medical Coverage Verification Errors Affect Cash Flow
Verification errors often trigger a domino effect on practice operations, ultimately impacting patient satisfaction. A single mistake during those eligibility checks can delay claims submissions, pushing back reimbursement by several weeks or months, stretching accounts receivable while also increasing staff burden. Those mistakes force staff to spend time identifying and correcting errors before resubmitting claims, calling payers and more.
While one error might not seem like a huge deal, multiple errors accumulate, reducing cash flow predictability and preventing practices from investing in growth.
Meanwhile, those delays affect patients. Unexpected bills, delayed services and other issues erode trust. Additionally, the decreased operational efficiency of your practice can result in lengthy wait times, excessive paperwork and an overall unsatisfactory experience.
The Hidden Costs of Manual Verification Processes
Many practices view manual medical coverage verification as inherently more cost-effective. Why pay for automated benefits verification tools when you could just have your staff do it all? The truth is that there are several hidden costs to manual verification.
As mentioned earlier, staff can spend well over six hours daily verifying insurance eligibility when using manual workflows. For larger practices and healthcare organizations, it can take even longer. The staff costs alone are substantial. When you factor in the time and effort involved to rework claims, hidden costs increase. Those hours spent calling payers, identifying errors and resubmitting claims add up, costing practices $25 to $118 per reworked claim.
Manual insurance verification comes with many upfront and hidden costs that can be difficult to quantify. However, they're not insignificant. Compare that with more efficient coverage verification software, and the difference is night and day. Automated insurance verification can reduce the average timeline from 13 minutes to just 30 seconds. Furthermore, automated software dramatically reduces the risk of error, virtually eliminating the time and costs of reworking denied claims.
Practices that switch to insurance verification software can see a return on that investment in just a few months, with measurable financial gains over the long haul.
Proven Solutions to Streamline Your Benefits Workflow
Modern solutions are turning the tide for practices of all sizes. Technology is changing the way that practices approach benefits verification. Automated software eliminates the need for hours of manual work, instantly checking eligibility, benefits, prior authorization requirements and more.
Coverage verification software takes only a fraction of the time required for manual processes while also preventing errors that can ultimately lead to denied claims. They can streamline the process from start to finish, and well-trained staff can leverage the technology to work more efficiently while delivering a better patient experience.
Implementing Automated Benefits Verification Systems
Automated tools perform real-time eligibility checks while seamlessly integrating with your existing systems. These systems reduce the need for manual entry, significantly decreasing the risk for errors and cutting back the time staff spend calling payers or looking up data in portals. Integration with your existing EHR and practice management systems further streamlines workflows, ensuring data flows into scheduling and billing without issue.
From an efficiency standpoint, automated benefits verification platforms can transform your practice. With less time spent on manual processes or correcting errors, these systems reduce administrative burden. Your practice can benefit from faster claim submissions, far fewer denials and more predictable cash flow.
Choosing the Right Coverage Verification Software
There are many options available for healthcare practices, but they're not all created equal. Here are a few key features to look for in a coverage verification software:
• Integration Capabilities: Your real-time benefits verification software should work with existing systems. The best options won't require additional software or require switching EHR systems.
• User Friendliness: An intuitive platform will ensure staff adoption and simplify training requirements, ensuring your entire team can leverage the software's capabilities.
• Scalability: The best software will offer full scalability, growing with your practice as your needs evolve.
• Comprehensive Reporting: Platforms should provide all the information about patient insurance coverage your practice needs, including verification at the CPT level.
Best Practices
Smooth, error-free insurance verification requires consistent workflows. Train staff to maximize the benefits of coverage verification software, establishing well-defined processes that everyone can follow. Avoid assigning verification duties to a single person. Having multiple staff members capable of performing verification can optimize efficiency across the board. Assign clear responsibilities and utilize standardized checklists that your team can follow consistently for every patient.
To avoid surprises, verify insurance coverage before every patient visit and update the data with each subsequent visit. For more complex scenarios, such as dual coverage, pending authorizations or sudden policy changes, create a clear escalation path that your staff can follow. Doing so will reduce errors and accelerate claims submission, allowing your staff to spend more time focusing on patient care and less time wasting resources.
Transform Your Practice Today!
Ready to transform your practice with automated benefits verification? Fuse is an end-to-end solution that can dramatically reduce errors, denials and reimbursement delays. Get real-time verification of a patient's benefits, without calling payers or using their portal. Fuse does it all for you, reducing the time administrative teams spend on verification by up to 95 percent.
With seamless adaptability that caters to your practice's workflows, implementing Fuse is easier than you might think. Most practices transition to Fuse in just a few days. Schedule your Fuse demo today to say goodbye to insurance verification challenges that negatively impact your practice.
Overcoming Healthcare's Biggest Insurance Verification Challenges
For many patients, the intake process they endure is the first real test of healthcare practices. According to recent surveys, 61 percent of Americans find the healthcare system a hassle for them, and another 71 percent reported major frustrations through their experiences with providers. Unfortunately, many go into these visits expecting the worst, only for practices to prove them correct.
Lengthy wait times, mountains of repetitive paperwork, unclear instructions and an overall outdated patient intake process sour the experience. The average patient takes 15 to 20 minutes simply completing forms, with first-time visits often requiring more time to go through a longer patient registration process. It's among the most frustrating parts of a visit. But that's not all. Delays caused by errors, duplicate data and more can put practices like yours behind, causing patients to wait as much as 41 minutes from completing registration to actually seeing a provider.
These complications set the stage for a frustrating experience that not only inconveniences patients but also increases workload for your staff. Practices seeking to stand out and create a more patient-focused experience must streamline patient intake and minimize friction from the jump.
Why Digital Patient Intake Solutions Drive Better Outcomes
Transitioning from paper to digital healthcare patient intake processes has become a key strategy for practices looking to improve patient experiences. Recent surveys suggest that a vast majority of patients are willing to complete forms digitally. Approximately 68 percent prefer it. While roughly half of patients still want to schedule appointments over the phone, most prefer the convenience and speed of digital patient intake.
Moving toward digital processes offers numerous benefits. The most obvious is speed and efficiency. Patient intake software can save practices up to 15 minutes per patient, significantly reducing wait times and patient frustration. Digital processes also improve patient experiences by offering flexibility. Patients can complete forms before they visit the clinic, even using mobile devices to finish the process. You can prevent front-desk bottlenecks while patients enjoy significantly shorter wait times.
That's not all. Digital systems also help improve accuracy. Old paper forms are prone to illegible handwriting, missing information and errors during manual data entry. Going digital can reduce errors by 60 percent, which helps save time, money and administrative burden for other downstream processes, such as insurance verification, claims submission, billing and collection. Modern intake software solutions also integrate seamlessly with EHR and practice management systems. That connectivity ensures effortless data flow between systems. It ultimately improves accuracy and reduces instances of duplicate data, facilitating smoother scheduling, billing and care coordination.
Streamline Patient Intake: 5 Proven Implementation Strategies
Streamlining patient intake doesn't have to be complicated. While it does require some preparation and staff training, there's much that you can do now to start seeing improvements across the board. Follow these steps to implement strategies that make a difference for patients.
• Send Pre-Appointment Digital Forms: allow your patients to complete intake forms digitally before their visit. After scheduling appointments over the phone and having them scheduled in the EHR, you can send them a link to start the patient registration process. Identify which forms patients can complete digitally, use patient intake software to create them, and configure systems to automatically send patients a link to complete them before their appointment.
• Send Automated Appointment Reminders: Automatic appointment reminders can keep patients engaged while reducing no-show rates and cancellations. Reminders also help staff manage schedules more effectively. Set text, email and phone reminders in your patient intake software. Then, customize messaging with appointment details and branding before scheduling reminders to go out one to three days before appointments.
• Provide Mobile Check-In Options: Mobile check-in gives patients a quick, contactless way to confirm arrival without requiring manual work from your administrative staff. Enable mobile check-in features in your patient intake software and provide clear instructions on what patients should do upon arrival to keep your office running smoothly.
• Train Your Staff: Front-desk staff need to understand how to use digital patient intake solutions. Provide ample training about software and tools, and teach your team how to guide patients through your new digital intake workflows.
• Collect Feedback and Optimize: Collect input from patients and staff. Accept feedback and monitor relevant metrics. The goal is to identify pain points and areas that need improvement. Refine your processes and ensure your new strategies continue to benefit your practice and patients.
Technology Solutions That Enhance Patient Registration Experience
Technology continues to reshape healthcare, and the right solutions can streamline patient intake in ways you never thought possible.
• Tablet-Based Check-Ins: Self-service kiosks equipped with easy-to-use tablets allow patients to check in upon arrival, confirm information, sign verification forms and more.
• QR Codes: QR codes offer a quick, easy and contactless way to check in and complete necessary forms on their own devices.
• Automatic Insurance Verification: This technology confirms eligibility in minutes, eliminating the need for manual checks while reducing errors and claim denials. Automating this process can cut back verification times by 90 percent per patient.
• Payment Processing Integration: Seamless integration allows patients to make secure payments during check-in, covering copays, outstanding balances and more. This integration provides convenience and may help improve collection rates.
• Online Scheduling: While many patients still prefer to schedule appointments over the phone, those who don't will benefit from the simplicity of online scheduling and automated reminders.
• Facial Recognition: Facial recognition and ID-scanning technology can quickly verify identities, pulling up EHRs instantly.
Adopting new technology can be daunting. There are always concerns about privacy, data security and patient adoption. While younger, tech-savvy patients tend to lean into digital patient intake technologies, older patients often hesitate the most. To ease those concerns, practices can provide options, including fully digital patient intake, traditional paper workflows or assisted intake with your staff. Post signage in your office with clear instructions on how patients can take advantage of your practice's new technologies. For older patients needing assistance, staff should be readily available to guide them through the process, answer questions and champion your practice's new digital initiatives.
Essential Patient Intake Software Features for Modern Practices
The right patient intake software solution can improve workflows, save your practice time, reduce data errors and create a far better experience for patients. However, with many options available, practices need to do their due diligence and find software that meets the mark. Here are several essential features and capabilities that your healthcare patient intake software should have.
• HIPAA Compliance: Software needs to protect personal health information (PHI), ensure full HIPAA compliance and help your practice avoid violation penalties. Look for end-to-end encryption, secure data storage, audit trails and user access control.
• Customizable Forms: Software should allow your practice to build fully branded, specialty-specific forms that capture relevant information without clutter or redundancy.
• Multi-Language Support: Multi-language patient registration processes ensure accessibility. The ability to complete forms and tasks in a patient's preferred language will reduce confusion, minimize the risk of errors and enhance the overall experience.
• Analytics Dashboards: Real-time reporting on wait times, form completion rates and more will help monitor practice performance while identifying areas in your patient intake process that require improvement.
In addition to the features above, your software should integrate seamlessly with existing EHR and practice management systems. Pre-built integrations and flexible APIs can facilitate smooth interoperability, allowing data to flow between platforms without issue.
When evaluating software operations, keep these features in mind. Reach out to vendors to learn more about software options and request live demos to see solutions in action. Consider upfront implementation costs, timelines, staff training requirements and ongoing subscription costs. Many practices find that while implementation takes time and adjustment, the right software pays for itself quickly through reduced administrative burden, better data quality and happier patients.
Healthcare Patient Intake Automation: Reducing Staff Workload
One of the most transformative features patient intake software can bring to the table is automation. Automation relieves overworked staff by doing much of the heavy lifting, replacing repetitive data entry tasks with seamless digital workflows. In addition to simplifying things for staff upfront, automation can improve data accuracy, preventing reworks, corrections and headaches later.
Automatic data population pulls information from submitted forms into a patient's EHR, preventing duplicate information and human error during manual data entry. Automating data entry reduces the risk of errors by 60 percent or more. One study found that practices using automation to populate data to EHRs cut error rates by 70 to 80 percent.
Automating insurance verification with real-time eligibility checks confirms coverage in seconds, saving around 15 minutes per patient and up to five hours of staff time per day. Meanwhile, automatic appointment reminders save staff hours on the phone while improving no-show rates by as much as 30 percent.
Of course, capturing these benefits for your staff requires training and buy-in. Before implementation, have your team complete a comprehensive onboarding program. This training will help staff learn how to navigate automatic systems, read relevant dashboards and support patients during the transition. Offer transparency and clear communication. To make things easier, consider transitioning to new software in stages. Implementing each automated feature one at a time will make it easy to move into new administrative workflows.
Measuring Success: KPIs for Your Patient Intake Process Improvement
Improving the patient intake process will be an ongoing effort, and your practice must track various metrics to continually push for positive change. To measure the success of your new patient registration process, monitor the following KPIs:
• Patient Satisfaction Scores
• Check-In Completion Rates
• Average Wait Times
• Time Spent Per Patient
• Data Accuracy
• No-Show Rates
Benchmark these metrics against industry standards to measure success and set realistic standards. See where your practice stands now and understand what areas you want to improve most. Be realistic about the changes you want to see and establish incremental goals. While patient intake software can make a considerable difference, transformations don't happen overnight. Drive progress by pushing for incremental improvements across these metrics and more.
Create accountability for your team. Review metrics frequently, identify what needs to change and implement corrective action to make it happen, all while supporting your staff every step of the way.
Improving the patient intake process will be an ongoing effort, and your practice must track various metrics to continually push for positive change. To measure the success of your new patient registration process, monitor the following KPIs:
• Patient Satisfaction Scores
• Check-In Completion Rates
• Average Wait Times
• Time Spent Per Patient
• Data Accuracy
• No-Show Rates
Benchmark these metrics against industry standards to measure success and set realistic standards. See where your practice stands now and understand what areas you want to improve most. Be realistic about the changes you want to see and establish incremental goals. While patient intake software can make a considerable difference, transformations don't happen overnight. Drive progress by pushing for incremental improvements across these metrics and more.
Create accountability for your team. Review metrics frequently, identify what needs to change and implement corrective action to make it happen, all while supporting your staff every step of the way.
Improve Satisfaction Rates with Proven Digital Patient Intake Solutions
Creating a better patient registration and intake process is no longer optional. Patients expect something better. Old-school approaches won't cut it. Fortunately, you can leverage technology to make changes that count. Software solutions like Fuse can streamline patient intake in many ways. Create a patient-friendly digital experience, automate tasks like insurance verification, establish simpler registration workflows and more. With Fuse, you can say goodbye to overworked staff, incomplete forms, frustrating data errors and other intake complications.
Give your patients the convenience they deserve, reduce the burden on your staff and gain a competitive edge that sets your practice apart. Request your Fuse demo today to learn more and see what digital patient intake can do for your practice.
Transform Healthcare Delivery: Essential Strategies to Improve Patient Experience During Intake
In the United States, healthcare providers spend roughly 30 percent of their operating budgets on administrative activities alone. Recent surveys suggest that the average medical intake process costs up to $23 per patient. Multiply that by thousands of patients annually, and inefficient medical intake workflows are costing practices big. However, what's more worrying is how outdated processes are resulting in widespread patient intake mistakes.
Simple mistakes, such as inaccurate data entry and incomplete information, can create unnecessary delays and preventable barriers to successful patient care. According to the World Health Organization, up to half of all medical errors in primary care are a result of administrative missteps. Some research suggests that 30 percent of medical claim denials are due to imprecise patient data.
Not only do healthcare provider intake errors cost providers time and money to correct, but they can also impact patient safety. Fortunately, these mistakes are entirely avoidable with the right system and ample training. Keep reading to learn more about the five most common mistakes made during the medical intake process and how your practice can avoid them.
Why Patient Intake Accuracy Matters More Than Ever for Healthcare Providers
Modern healthcare relies heavily on data, and regulatory compliance requirements are putting a heavier burden on practices and providers. The HITECH Act expanded security regulations under HIPAA, creating more compliance requirements for electronic health record intake systems. These new regulations aim to enhance data quality, minimize patient registration errors and improve patient safety. Providers must be more vigilant about avoiding mistakes to comply with regulatory standards while also ensuring patient safety.
Patient intake mistakes compromise safety in many ways. Incorrect data can lead to misdiagnoses, improper treatments, medication errors and delays in care. These mistakes can affect the quality of care that patients receive, potentially having life-changing impacts. But that's not all.
Because healthcare intake forms directly affect billing, insurance claims and reimbursements, mistakes can result in lost revenue. Claim denials reportedly cost hospitals and health systems nearly $20 billion a year! With a significant percentage of denials being caused by data errors, the need for improved workflows and rock-solid patient intake software is at an all-time high.
Mistake #1: Incomplete Medical History Collection
One of the most common healthcare provider intake errors that affects patient care and safety is incomplete data about an individual's medical history. Rushed medical intake workflows leave little time for patients and administrators to paint the whole picture. While many focus solely on basic identification data and insurance information, providers need to understand a patient's medical history to provide efficient care.
Without that critical information, providers can make grave mistakes when diagnosing a patient's condition. That lack of data can also lead to incomplete or potentially harmful treatment plans. For instance, some common bits of information that rushed intake processes miss include allergies, drug sensitivities and psychological health concerns. Without that information, providers can inadvertently develop treatment plans that actively harm patients.
Best Practices for Comprehensive Medical History Forms
Healthcare intake forms and processes need to be comprehensive. No matter how rushed practices are, there are several sections your medical history forms should never skip. These include:
• Allergies
• Medications
• Previous surgeries
• Family histories
• Chronic conditions
• Immunization status
These details all help healthcare providers treat patients successfully. Medication reconciliation and information about allergies will inform providers about what to avoid. Meanwhile, family medical histories can help providers understand a patient's unique risk factors.
Urging patients to provide complete information without skipping sections can be challenging, especially in a rushed environment. Patient intake best practices recommend giving individuals ample time and flexibility. Provide options on how patients can provide necessary data, including self-administered forms or verbal disclosure. Administration should communicate the importance of providing this critical information, all while remaining sensitive to a patient's need for privacy.
How Technology Improves Healthcare Intake Forms Accuracy
Technology can transform your entire medical intake process. Patient intake software digitizes the process, helping prevent errors and omissions that could impact care. Digital forms with validation are an effective way to ensure that the information gathered is accurate. User-friendly processes force patients to double-check the information provided, dramatically reducing errors. When integrated with EHR systems, digital forms make a difference.
Features like automated reminders can also prevent incomplete sections, encouraging patients to provide all relevant information about their medical history, medications, allergies and other pertinent details.
There are countless benefits to implementing technology into your patient intake workflow. However, the most significant is that patients can provide critical information on their own terms. Patients can complete forms at home before their visit, rather than spending 20 minutes rushing through them in the office.
Mistake #2: Poor Insurance Verification and Patient Registration
Insurance errors are another administrative headache that costs providers billions annually. The financial impact is monumental. Patient registration errors often lead to denied claims, which impact both providers and patients. Insurers that offer plans on the Health Insurance Marketplace deny nearly 20 percent of in-network claims and 37 percent of out-of-network claims, and a significant percentage of those denials are due to poor insurance verification. Almost 27 percent are a product of eligibility issues.
Each processing error reportedly costs providers up to $125 to identify and correct, with claims adjudication costing providers over $25 billion annually. On top of all that, patient billing disputes significantly increase administrative costs.
Insurance verification should be a top priority during the patient intake process. Verification should occur before a patient even steps foot in the office. By verifying insurance information and eligibility before a visit, practices can avoid denied claims and ensure patients have coverage before rendering treatment. Waiting until after a patient's visit will only increase the risk of denials and disputes.
Streamlining Patient Registration Process for Better Outcomes
Many practices use patient intake software, but they often fail to complete adequate insurance verification. While many promise to check eligibility, they don't do so accurately, forcing many practices to turn those features off entirely.
Patient intake best practices involve step-by-step verification processes. Software should effectively perform real-time eligibility checks, ensuring everything is in order before a patient's office visit. Patient intake software should also collect backup insurance documentation to prevent delays in care and over-complicated claims processing.
The best software utilizes AI to automate these tasks, freeing up staff and streamlining the registration process from the outset.
Mistake #3: Inadequate Staff Training on Medical Intake Workflow
Undertrained staff can create bottlenecks in your medical intake processes. Administrative teams need to operate like a well-oiled machine. Otherwise, the process can be a nightmare for healthcare providers and patients alike.
As bottlenecks develop, staff will have no choice but to rush through the process. The result is an increase in data entry errors and a lack of consistency. Training gaps in HIPAA compliance may also elevate your risk of data breaches, penalties and reputational damage.
A lack of training for administrative personnel can harm your practice in countless ways. It has a ripple effect, compounding patient frustration and leading to more patient intake mistakes that require time and money to correct. Furthermore, neglecting comprehensive training can lead to high turnover rates, which in turn add further confusion and chaos.
Essential Training Components for Patient Intake Teams
Every member of your administrative team needs thorough training. Successful patient registration processes require strong verbal communication skills, active listening and a deep understanding of how to avoid potential errors. Teams also need HIPAA compliance training and education about insurance verification processes.
Training can be time-intensive and costly. Furthermore, even with ongoing efforts to improve skills and workflows, errors are still possible. Practices like yours should consider automation. Patient intake software that can handle more complex administrative tasks will improve efficiency, reduce manual errors and allow administrative teams to focus on serving patients in other ways.
Mistake #4: Lack of Quality Control and Error Tracking
Combating patient intake mistakes is a constant battle for practices. One study found that over 20 percent of patients identified errors in their own medical records. That's just including patient-reported issues. Those that go unnoticed until they create patient care or insurance processing issues are likely far higher.
Many patient intake processes lack quality control and error tracking. As a result, mistakes slip through the cracks. Successful quality control requires a multipronged approach. However, automation can do much of the heavy lifting, removing the burden on administrative staff. Modern patient intake software can automate error tracking entirely; practices need to take advantage of these capabilities.
Implementing Effective Intake Quality Assurance Programs
Quality assurance programs and automation can make a world of difference. Successful implementation is about understanding the types of errors that impact your practice and developing strategies to avoid them. Error tracking systems can help identify issues early on, allowing providers and administrators to address them before they impact patient care. Meanwhile, regular audits can scrutinize current medical intake workflows and highlight areas that require improvement.
Quality control is a data-intensive process, and there are many metrics that practices should track to monitor potential patient intake errors. Data should be the driving force for change. Audits can highlight challenges, enabling providers to easily identify training needs and system improvements that can foster positive change. Some key metrics to track include:
• Patient data accuracy rates
• Claim denials
• Correction time
• Missing form rates
• Missing identification data
• Audit failure rates
Mistake #5: Outdated or Inefficient Patient Intake Software Systems
Inadequate software is a bigger source of patient registration errors than most providers realize. Technology in the healthcare space is nothing new. Practices have utilized software to streamline patient intake for decades. However, legacy systems aren't capable of keeping up with modern demand, and many older software tools create more work than necessary.
Dated software can lead to more errors, frustrating both staff and patients. Inefficient workflows and inoperability issues can create more problems than the software claims to solve.
Poor EHR integration is a common problem with older software programs. Inconsistent data formats and a general lack of data standards often lead to omissions and errors. Weak integration can also create manual data entry problems. Older patient intake software may even lack robust security protocols, creating vulnerabilities and concerns regarding HIPAA compliance.
Legacy systems are a byproduct of a time when automation was lean. As a result, many intake providers simply don't have the capabilities that modern healthcare providers need. For example, many don't perform insurance eligibility checks and lack any automation features that can truly streamline your medical intake workflow. Some don't even have features that allow you to customize forms to match your practice's branding.
Key Features to Look for in Modern Healthcare Intake Solutions
Upgrading your patient intake software can take your workflow into the 21st century, helping your practice work more efficiently while avoiding errors that can negatively impact your business and the patient experience. While many providers hesitate to make such a significant change, investing in new patient intake solutions can deliver a high ROI.
The right software can greatly reduce administrative costs and lower insurance claim denial rates. Those benefits create a less stressful experience for patients, ultimately improving your practice's reputation and bottom line. While implementing new software can be daunting, the investment is well worth it. Depending on the size of your practice, implementation can take as little as a few weeks. You can get up and running in no time, moving toward a more efficient and error-free future.
So, what features should providers look for in patient intake software?
•Smooth EHR Integration: Proper EHR integration can save your staff time and eliminate the need for manual data entry. With integration, software can automatically populate a patient's EHR with data.
•Automation: Automated workflows simplify the medical intake process. Automation can create a digital experience that helps your practice capture all relevant data while reducing your administrative burden.
•Real-Time Insurance Verification: Real-time verification eliminates delays, errors and denials. You can verify insurance eligibility before administering care, all without the error-prone manual processes.
•Mobile Compatibility: Mobile compatibility allows patients to complete forms anytime, anywhere. Ditch paper forms and give patients more freedom to provide the information your practice needs.
•Analytics and Reporting: In-depth analytics and comprehensive reporting help you track errors and highlight inefficiencies that could impact your practice.
Transform Your Patient Intake Process with Proven Solutions
Patient intake mistakes don't have to cost your practice. Administrative costs are already at an all-time high for providers like you. Simple errors during the medical intake process create additional costs and delays, sacrificing the patient experience while putting their safety at risk.
The mistakes we mentioned are entirely avoidable. All it takes is the right patient intake systems and proper staff training. Fixing these mistakes with an end-to-end patient intake solution can lead to lower administrative costs, fewer error-caused claim delays and far better patient outcomes.
Fuse offers complete healthcare automation, streamlining the patient intake process while performing CPT code-level insurance verification. Prevent errors, eliminate the stresses of complicated intake processes and free up time to allow your team to focus on patient care. Schedule your Fuse demo today to learn more and see firsthand how an automated medical intake process can benefit your practice.
5 Critical Patient Intake Mistakes That Cost Healthcare Providers Time and Money
In the world of healthcare, trust is everything. However, many patients find it difficult to trust their medical providers, and a significant part of this is due to a lack of transparency. One survey found that around 41 percent of respondents believed that their healthcare providers weren't being transparent about the costs of their medical care. That's a significant issue that practices should work to resolve.
Numerous studies show that medical bills are a major source of stress and anxiety for patients. One study suggested that more than half of patients find medical bills a top source of stress. Another found that 34 percent of respondents have lost trust in providers due to an overwhelming and stressful billing experience.
Better healthcare price transparency can help alleviate that anxiety, paving the way for an informed and confident patient experience. A recent study showed that patient fee transparency has a measurable impact.
As a healthcare provider, it's vital to provide accurate and transparent medical cost estimates. In addition to doing better by your patients, healthcare billing transparency can help ensure that your practice complies with all Centers for Medicare & Medicaid Services (CMS) requirements, including those for good faith estimates.
In this blog, we'll explore how transparent pricing in healthcare makes a difference and how your practice can take steps to provide more accurate estimates for patients.
The Direct Connection Between Healthcare Price Transparency and Patient Satisfaction
Patients care about healthcare price transparency, and it frequently affects their loyalty to providers. In one study, 40 percent of respondents stated that they would delay or cancel care appointments if they didn't receive cost estimates beforehand. Other studies found that up to 60 percent of patients will seek care elsewhere if pricing and billing aren't up to par. Transparency significantly impacts patient satisfaction, and that's not just hearsay.
For one health system, a shift to what some called "radically" transparent medical cost estimates proves just how much patients care about understanding healthcare costs. When this health system began providing unprecedented access to pricing information, its patient satisfaction healthcare rates rose to 82 percent in just one year.
For the average patient, pricing remains a mystery. In one survey, 68 percent said they don't know how much an appointment will cost until months afterward. When they eventually do receive a bill, 61 percent said that it was more confusing than a mortgage payment!
Transparency matters, and it's clear that a lack of it will negatively impact patient satisfaction. It's not difficult to see why. Those unknowns are stressful, and surprise bills can erode trust with providers faster than most realize.
By prioritizing accurate and open patient cost estimates, practices can mitigate the risk of unexpected costs, foster trust and reduce patient anxiety. That transparency also helps with better treatment compliance while dramatically improving patient-provider relationships and ultimately enhancing patient retention.
Why Patient Fee Transparency Matters More Than Ever
The healthcare landscape continues to transform, not just in terms of regulatory requirements but also in patient expectations. Patient satisfaction in healthcare is always a top priority, and pricing transparency is emerging as a crucial factor that influences the success of healthcare practices.
In a post-pandemic world, patients are increasingly seeking clarity in pricing. According to one study, 69 percent of patients are interacting with providers differently than they were pre-pandemic, with 71 percent wishing that the experience was as easy as other areas of their lives. Another found that 9 out of 10 patients now want to know their payment responsibilities upfront.
On the regulatory front, health plans and hospitals have a legal obligation to provide pricing information. CMS requirements aim to promote healthcare price transparency, enabling patients to compare prices and make informed decisions about their care. New regulations went into effect in 2025, and rules surrounding transparency continue to evolve.
Failing to comply could lead to penalties. Furthermore, a lack of transparency could harm a practice's reputation and ability to retain customers. Healthcare providers and practices that embrace transparency encourage patients to remain loyal, even as healthcare costs rise. With an estimated 94 percent of Americans supporting transparent pricing in healthcare, failing to meet the mark could cost your practice. Alternatively, going above and beyond gives your practice a competitive advantage.
Implementing Transparent Pricing Healthcare Solutions in Your Practice
Providing transparent patient fee estimates is more challenging than most realize. According to a recent audit by a patient advocacy group, just 21 percent of hospitals in the U.S. were complying with new federal rules. Complying with new regulations and meeting patient expectations requires a structured approach. Here are a few steps that practices can take:
•Define Your Objective: Start by identifying your goal in providing patient fee estimates. For most practices, the ultimate objective is to offer estimates upfront, before patients arrive at the clinic. That should take precedence, as early upfront information can significantly reduce billing department calls while also streamlining collections. It ensures patients understand their financial obligations from the jump, which helps prevent collection failures.
•Understand Payer Contracts: When implementing transparency strategies, practices must fully understand payer contracts. Review contract information thoroughly. Practices need to know whether they're in-network for a patient's insurance and what "allowed amounts" apply. Otherwise, providing accurate medical cost estimates on a per-patient basis becomes near impossible.
•Adopt Tech Solutions: There are ways to provide estimates manually. For instance, administrators can create spreadsheets with allowable amounts by CPT code and payer plan type. That cheat sheet can help develop estimates, but it still requires significant manual labor that could lead to errors. The best way to save time and effort is to adopt tech solutions that automate that process. Software like Fuse can automatically calculate fee estimates in minutes, removing some administrative burden while providing more accurate figures.
•Integrate Tools with Practice Management Systems: When leveraging digital tools, they should integrate with EHR and practice management systems. Seamless integration helps simplify workflows and reduce errors. These tools and systems can share data to improve accuracy and save time.
•Invest in Staff Training: Staff training is pivotal. Teams need to know how to provide accurate estimates, use applicable tools and communicate information to patients. It's also wise to ensure that everyone is familiar with transparency requirements to help maintain compliance.
Best Practices for Medical Cost Estimates and Patient Communication
Beyond those steps to implementation, there are many patient fee transparency best practices to follow.
•Timing: Timing matters. You want your patients to understand relevant costs before you administer treatment. The best approach is to provide patient cost estimates before their visit. Early disclosure can ease worries and reduce cancellations. It builds trust from the start and provides ample time for patients to ask questions if necessary.
•Format Preferences: There are many ways to communicate cost estimates. The best option is to provide standardized documents. Use plain language and avoid complicated medical jargon. Documents should include itemized costs whenever possible and utilize visual aids to facilitate understanding. Forms should be accessible via digital formats for early delivery.
•Follow-Up Communications: Transparency doesn't end upon estimate delivery. Provide follow-up reminders and encourage patients to reach out. Include contact information and emphasize your practice's commitment to transparency and patient-focused care.
•Consistency: Finally, ensure medical cost estimates are consistent across digital portals, phone calls, in-person communications, etc. Different figures will only erode trust. Using digital tools to automatically calculate fee estimates can help with data inaccuracies that lead to discrepancies.
Overcoming Common Patient Fee Estimates Implementation Challenges
There's a reason why audits find compliance to be so low. There are many challenges to providing transparent pricing in healthcare.
One is insurance complexity. Different payers have varying rules and restrictions, which often makes it difficult to provide accurate estimates. Here's where a thorough understanding of payer contracts, combined with the use of automation, makes a significant difference. Insurance verification and fee estimate tools can cut through the confusion, providing accurate data for every patient.
Varying costs for specific procedures and treatments also come into play. Practices can overcome this challenge by creating standardized pricing templates. Strong communication with patients is also vital. Explaining some of the pricing variability can help minimize disputes and avoid significant billing surprises.
Finally, staff resistance to healthcare price transparency can impact implementation. Many see transparency efforts as increased workloads and greater risks of mistakes. However, you can alleviate those concerns by using the right digital tools. Software can do much of the heavy lifting, actually saving administrators time while also reducing patient complaints and improving collection rates.
The best way to implement new strategies is to do so in stages. Phased implementation can ease your practice into a better way of doing things. Consider adopting techniques and workflows slowly. Doing so will allow your practice to measure success, make improvements and ensure positive results.
Measuring Success: Healthcare Billing Transparency Impact on Practice Metrics
Measuring the success of your new transparency efforts can prove their value to stakeholders. There are several metrics to monitor. These include patient satisfaction in healthcare scores, billing dispute rates, collection efficiency, pre-visit inquiries, patient retention rates, no-show rates and more.
As you measure these metrics, you'll quickly see how a dedication to transparent pricing in healthcare makes a difference. The ROI potential is significant. When presenting the value of your initiatives to stakeholders, highlight the impact on revenue and patient satisfaction. You can also emphasize changes in operational efficiency, showing how your efforts are making things easier for staff across the board.
Transform Patient Experience with Clear Fee Communication
Transparent healthcare pricing is more than just a regulatory requirement. It's also a competitive advantage that can help boost your patient satisfaction scores, improve retention and create an overall better experience for patients. Trust is the foundation of any strong patient-provider relationship. Transparency about healthcare costs is a massive step in the right direction.
Fuse can help you streamline the estimate process, providing greater transparency and more accurate numbers than ever before. With Fuse, you enjoy automated calculations, real-time insurance verification, impression integration capabilities and more. Use Fuse to improve patient engagement, increase your practice's operational efficiency and gain that competitive edge you need to reach the next stage of success.
Schedule your Fuse demo today to learn more and see how automated patient fee estimates can transform your practice.
How Transparent Healthcare Pricing Drives Patient Fee Transparency Success
Medical insurance verification can be a burdensome process, but it's unavoidable. While most medical providers want nothing more than to focus solely on patient care, verifying insurance eligibility is crucial for protecting a practice's revenue and ensuring that patients can access treatment.
Outdated manual processes are notorious for being time-consuming and frustrating. On average, practices reportedly spend more than 12 minutes manually verifying a single patient's insurance eligibility. In some cases, verification can take as long as 60 minutes when including holding time when calling payers. That might not sound like much, but that time adds up when you consider how many patients your practice sees daily. That's not all.
Manual data entry significantly increases the risk of error, and that can cost your practice even more time and money. Human error rates in manual data entry can be as high as 5 percent, and those mistakes are reportedly the cause of 25 percent of claims denials. Errors are expensive, costing practices upwards of $50 to reprocess a denied claim. Furthermore, mistakes can disrupt the healthcare revenue cycle, delay care and harm the overall patient experience.
It's not hard to see why medical providers are searching for better alternatives to outdated manual insurance verification methods. Luckily, modern tech solutions can address those frustrations and more. Technology is revolutionizing insurance eligibility verification, leading to greater practice efficiency, more patient satisfaction and even better outcomes. Read on to find out how.
The Power of Automated Insurance Verification for Medical Practices
Automated medical insurance verification can transform your practice's entire approach, saving valuable time and effort while dramatically reducing the risk of error. Insurance verification technology takes much of the manual work out of the equation. As a result, you can verify a patient's eligibility faster and more accurately, reducing staff burden while improving the patient experience.
Real-time insurance verification can cut that industry norm of 12 minutes to verify a patient's insurance down to a fraction of this. Not only that, but it can also prevent claims denials. Real-time insurance verification works by connecting with insurance payers to confirm a patient's coverage, providing near-instant feedback. Software can alert you to missing or incorrect information, significantly reducing the risk of having to resubmit claims or rework forms.
Administrative staff can enjoy more streamlined workflows, and practices save significant time and money. According to the CAQH 2024 Index, automated insurance verification can save the medical industry a whopping $11.7 billion annually in administrative costs.
Essential Features of Modern Eligibility Technology Solutions
There's no shortage of options available to practices, but for insurance verification technology to truly streamline operations and reduce claims denials, solutions need to have a few key features.
•Real-Time Eligibility Checks: Performing eligibility checks at the point of service, or even before patients come in for an office visit, allows practices to catch discrepancies before filing claims. This feature can prevent error-based denials and help patients have a clearer understanding of their benefits upfront.
•EHR Integration: Smooth integration with electronic health record (EHR) systems ensures precise data flow between clinical and administrative workflows. Insurance verification software can populate EHRs with relevant data, eliminating the need for manual data entry and reducing the risk of errors.
•Batch Processing: High-volume practices can benefit tremendously from batch processing. Rather than checking eligibility on a patient-to-patient basis, you can run checks for multiple patients simultaneously, saving time and reducing administrative burden.
•Comprehensive Coverage Discovery: The best insurance verification solutions run eligibility checks to the CPT code level. CPT code-level verification enables providers to understand precisely which procedures a patient's policy covers, including any limitations or prior authorization requirements. The granular view of eligibility eliminates surprises, reduces denials and helps patients understand potential out-of-pocket costs.
•Multi-Payer Connectivity: Verification solutions should work with major commercial insurers and government programs like Medicare and Medicaid. Comprehensive payer connectivity can automate verification workflows and provide more detailed information about a patient's coverage, even if they have eligibility from multiple policies.
Streamlining Insurance Eligibility Verification Workflows
Insurance verification technology can integrate seamlessly into existing practice management systems, automating workflows from start to finish while transforming patient intake processes. Automated insurance verification takes only minutes. After patients complete intake forms, the software can handle the rest to check eligibility before providers render any treatment or file claims. If your practice encourages patients to complete forms digitally before their visit, insurance verification can occur before they even enter your office.
Automated verification alerts you to potential issues and missing data, giving patients and administrators ample time to make corrections before dealing with payers. That simplified workflow benefits everyone. Front desk staff will spend less time chasing down patients or reworking claims. Meanwhile, patients enjoy a much speedier and less stressful check-in process. Automating insurance verification can cut back on patient wait times by 40 percent or more, resulting in greater patient satisfaction.
Enhanced insurance verification workflows can also impact the broader healthcare revenue cycle. In addition to reducing administrative work, automated processes pave the way to cleaner claims downstream. Accurate information and real-time eligibility checks translate to faster reimbursements, more predictable revenue and a better reputation among patients.
Real-Time Coverage Check Benefits
Standard manual insurance verification often requires administrative staff to have lengthy phone calls with payers. It involved navigating frustrating automated menus and waiting for available representatives, which wastes valuable time. Furthermore, those outdated processes often resulted in missed details.
Automated insurance verification solves many of those complications, pulling eligibility information in minutes with no need to make a phone call. Software also provides more comprehensive coverage discovery thanks to CPT code-level verification. Tech solutions highlight critical information about out-of-pocket costs, limitations, prior authorization requirements and more.
Patients benefit from greater transparency, as they fully understand their financial responsibilities before receiving any care. Meanwhile, practices receive more complete information, which leads to more accurate billing and fewer coverage surprises.
Medical Eligibility Technology Integration Strategies
The key to successful insurance verification technology implementation is smooth integration. When setting up software solutions, practices must ensure proper data flow and system connectivity. Verification software needs to work effortlessly with existing practice management systems while also sharing data with EHR systems. Optimized data flow enables staff to initiate verification checks without performing substantial manual data entry, thereby mitigating the risk of errors.
It's also vital to train staff to make the most out of insurance verification software. Proper training shortens the learning curve, gives staff the confidence needed to use the software to its full potential and turns software solutions into a driver of operational efficiency in your office.
Healthcare Automation Tools ROI Analysis
Medical insurance verification solutions are well worth the investment. While it can take time to integrate software into existing systems and train staff, the time and expenses spent transitioning to real-time insurance verification and automated workflows pay off over the long term.
Automated workflows eliminate the need for manual data entry, significantly improving accuracy. First-pass verification accuracy reportedly jumps to over 99 percent with automation, almost eliminating error-related claims denials. One study found that the number of denials caused by a lack of eligibility plummeted to under 2 percent of all claims.
Practices like yours can also enjoy a more predictable healthcare revenue cycle. Insurance verification technology reportedly reduces reimbursement time by around 50 percent.
Transform Your Practice with Advanced Insurance Verification Solutions
Outdated insurance verification processes should not get in the way of patient care. When you're ready to ditch the old manual workflows in favor of automated, real-time insurance verification, turn to Fuse. Fuse is an end-to-end solution that brings automation into your practice. In addition to improving the patient intake process, Fuse performs CPT code-level verification automatically.
Transitioning to advanced insurance verification software can save your practice time and money, all while giving you a competitive advantage as you create a smoother, frustration-free experience for patients. Reach out today to schedule a demo and learn more about how Fuse can transform your practice and boost your bottom line.
How Insurance Verification Software Transforms Healthcare Operations
According to the American Chiropractic Association, over 35 million people seek treatment each year. The field of chiropractic care is growing, but many practices struggle to find a balance between pushing for patient growth and adhering to ethical standards. Like any other practice in healthcare, effective marketing is paramount. Without marketing, providers can't maximize chiropractic patient attraction to reach the next stage of success.
However, there's a fine line between ethical chiropractic marketing and potentially deceptive or exploitive marketing. While the latter may attract more attention, ethical healthcare promotion has a more lasting positive impact.
One study found that patients are far more likely to choose a chiropractor who demonstrates ethical marketing practices and transparency. Practices that prioritize ethical marketing strategies, excellent patient care and maintaining strong relationships can reportedly achieve referral rates as high as 97 percent!
Keep reading to learn more about how your chiropractic practice can achieve growth through effective marketing without sacrificing your ethical standards.
Why Chiropractic Practice Marketing Must Prioritize Professional Standards
Ethical chiropractic practice marketing isn't optional. There are numerous professional standards that practices must adhere to. Failing to comply with those standards can be costly.
Regulatory oversight comes from state chiropractic boards and the Federal Trade Commission (FTC). Each state sets guidelines for ethical healthcare promotion, with most prohibiting unsubstantiated claims, misleading information or unauthorized use of official titles. For example, New York requires that practices refrain from scare tactics and deceptive communications. Meanwhile, Georgia prohibits the misrepresentation of facts and the creation of false expectations.
Breaking those rules could result in license suspension and steep penalties. You must familiarize yourself with what specific rules apply in your state.
FTC guidelines apply to all chiropractors across the country. Guidelines are expansive, but they include specific rules regarding the use of endorsements and testimonials, as well as the importance of providing scientific evidence to support all claims in marketing materials.
Applicable rules are complex, and there are many ways that professional chiropractic advertising can cross the line. Some common examples include statements like: "Guaranteed pain relief in one visit," or "Cure your back pain."
Even using exaggerated before-and-after photos, X-rays and other images designed to scare patients into seeking treatment crosses the line.
Practices must be careful about how they approach marketing. Not only can breaking applicable rules and guidelines lead to license suspensions and penalties, but they also erode patient trust. Your practice's reputation can suffer significant damage, potentially harming your business in the long term.
Building Patient Trust Through Compliant Healthcare Marketing Strategies
Trust is the foundation of strong patient relationships, and earning that trust begins long before an individual ever reaches out to create an appointment. Compliant healthcare marketing that's professional and ethical sets the stage, allowing you to establish trust from the outset. Doing so will make patients more confident in your practice's capabilities, ultimately translating to better retention and long-standing patient relationships.
Here are a few strategies that help build trust while adhering to chiropractic advertising standards:
•Always Use Evidence-Based Claims: Only make claims your practice can substantiate with evidence. Always cite sources and provide scientific data to back your claims.
•Offer Transparent Pricing: Clearly communicate costs and provide accurate estimates. Transparent pricing information reduces confusion, prevents surprise bills and improves patient satisfaction.
•Set Realistic Expectations: Set accurate expectations about outcomes and timelines. Avoid language that implies unrealistic benefits or miracle cures.
•Comply with All Testimonial Guidelines: Testimonials are powerful, but you must follow ethical guidelines. Always get authorization, disclose typical results and never incentivize patients to provide testimonials.
•Follow All Photo Rules: All before-and-after images must comply with state board and FTC rules. You should never alter photos, use them to scare potential patients or represent atypical results.
Ethical Chiropractic Marketing Channels That Drive Real Results
There are many ways to reach potential new patients while adhering to compliant healthcare marketing standards. These days, practices need a multichannel marketing strategy that leverages online visibility and offline outreach.
Digital marketing solutions include email marketing campaigns, social media posts and a well-optimized website. Through social media platforms, practices like yours can share wellness tips, patient success stories and more. Meanwhile, email campaigns can keep patients well-informed about treatment pricing, promotions and other relevant details about your practice. A great website also goes a long way, being the go-to source about your practice. Top-notch SEO practices can help improve visibility, making it easier for would-be patients to find your business.
Of course, you should also promote your practice outline. Community outreach programs, participating in professional referral networks and publishing educational content to teach people about what your practice does can help improve chiropractic patient attraction rates without sacrificing healthcare marketing compliance.
Professional Chiropractic Advertising Standards for Digital Platforms
We live in a digital-first world, presenting countless opportunities for chiropractic practices to reach massive audiences. While your practice should take full advantage of digital platforms, there are also many chiropractic advertising standards to follow. Not only does healthcare marketing compliance help you avoid penalties, but it can also build trust with potential clients before they ever seek treatment.
Let's dive into some essential guidelines you need to follow when publishing online content. For website content and social media posts, follow these rules:
•Avoid Unsubstantiated Claims: As always, everything you post needs to be truthful and backed by science. Provide evidence of your claims and make disclosures clear to avoid accusations of deception.
•Always Obtain Consent from Patients: When publishing testimonials, patient stories or images, always get consent and protect privacy to comply with HIPAA guidelines.
•Clearly Display Professional Titles and Credentials: When pushing content, make professional titles and credentials clearly visible. Doing so will build trust and authority.
•Be Careful About Photo Usage: Never alter photos. Like testimonials, gain patient consent and ensure that nothing you post is deceptive.
•Use Accurate Terminology: Use approved terms when describing services and treatments. Generally, terms like "chiropractic adjustment," "spinal manipulation" and "musculoskeletal care" are accurate and approved. However, refer to state guidelines. Some states have restrictions on chiropractors using terms like "functional medicine."
•Avoid Prohibited or Questionable Language: Don't use terms that misrepresent the scope of chiropractic medicine, and avoid language that claims you can "cure" or "heal" specific conditions.
Those rules apply to all digital content. However, there are also some platform-specific guidelines. Specifically, Google Ads limits have strict chiropractic standards. Before you can promote healthcare content, your practice must obtain proper Google certification. All content must also adhere to Google's healthcare advertising policies. Similar guidelines also apply if you publish content on Meta platforms, such as Facebook or Instagram.
Creating Compliant Content That Attracts Your Ideal Patients
Professional chiropractic advertising that complies with ethical standards can help you attract high-quality patients. Beyond traditional digital marketing, consider publishing content that educates and informs your audience. Doing so can help foster trust, all without needing to resort to unsubstantiated claims, empty promises or other questionable marketing tactics. That trust turns into long-lasting patient relationships and turns your practice into a trusted authority in chiropractic care.
•High-Value Blog Topics: Blog content shouldn't focus exclusively on marketing your practice. While high-quality content does that organically, aim to provide real value to potential patients. Consider publishing articles about ergonomics, spinal health, posture tips and more. You can even produce content that explains treatments and chiropractic adjustments. This type of content helps patients understand how chiropractic care supports their overall wellness and sets your practice up as a trusted resource for information.
•Informative Infographics: Infographics are highly accessible and easy to understand, even to those who are considering chiropractic care for the first time. Publish visually appealing infographics that explain spinal anatomy, safe movement techniques or exercises, common musculoskeletal issues, etc.
•Educational Video Content: Videos are another form of highly digestible content that can help you achieve ethical healthcare promotion. Videos about stretches, exercises and proper lifting techniques provide value to patients. Remember to include disclaimers, identify provider credentials and other healthcare marketing compliance standards.
•Useful Downloadable Resources: Resources that patients can use offline are always helpful. You can provide download links to exercise guides, office visit checklists, informative ebooks and more.
When creating this content, focus on educating patients about conditions and relevant treatments. Avoid making promises about cures or offering unrealistic claims. Lean into valuable insights and safe practices.
Ethical Healthcare Promotion Through Community Engagement
Online content and professional chiropractic advertising can make a difference. However, nothing compares to hands-on community engagement. It's all about meeting patients where they are, interacting with people in real environments and positioning providers at your practice as healthcare experts while staying compliant. Community engagement can be powerful, but what types of opportunities should your practice take advantage of?
•Professional Networking Events: Networking events allow healthcare professionals from all backgrounds and specialties to get together. It's an excellent way to meet others who may interact with patients. You can share your knowledge and receive referrals. If one of those healthcare experts meets a patient looking for a chiropractor, they may choose to refer you based on the interaction you had during one of these events.
•Health Fairs: Many communities throw health fairs. These events enable community members to receive treatment, undergo screenings and learn more about the healthcare options available to them. Participate as a vendor to share information and provide educational materials. Your chiropractors can even do spinal health demonstrations or posture screenings.
•Workplace Wellness Programs: Consider working with local employers. Many are looking to start wellness programs, and this presents an excellent opportunity to promote your practice. Your practice can offer educational workshops, wellness tips, ergonomic assessments and more. Engage with employers and focus on preventative care.
•Speaking Engagements: Host online or in-person seminars. Community events about musculoskeletal health, injury prevention and more are fantastic opportunities to educate people while establishing your practice as an authority on chiropractic care.
Transform Your Practice with Proven Ethical Marketing Systems
Developing a comprehensive marketing strategy that complies with all chiropractic advertising standards and ethical healthcare promotion guidelines is your practice's ticket to sustainable growth. Earning the trust of patients is more important than ever. With the right marketing strategies across digital channels and community outreach opportunities, you can attract and retain patients, earn their trust early on and safeguard your professional integrity.
Your efforts will pay off handsomely over the long term. Ethical chiropractic marketing can pave the way to sustainable growth, more practice revenue and reduced legal risks. Let Fuse be your growth partners. Fuse is an end-to-end solution that automates many healthcare administrative tasks, helping deliver accurate price estimates while transforming practice operations.
Reach out to schedule your Fuse demo today!
How to Attract More Patients Through Ethical Chiropractic Marketing That Builds Trust
Did you know that a vast majority of Americans value pricing transparency in healthcare? In a poll conducted for Patient Rights Advocate, 96 percent of voters across the political spectrum believe that healthcare consumers should have transparent patient fee estimates upfront. It's so important to patients that an estimated 40 percent are willing to cancel appointments or delay care if they don't receive healthcare payment estimates beforehand. Nearly half would switch providers for better upfront information about healthcare costs.
Upfront pricing estimates help to build trust with their providers. That transparency helps to alleviate the stress that patients feel about covering healthcare costs. Not only do estimates create a better patient experience, but they can also improve the likelihood that patients will make payments.
One provider in New York implemented a transparent billing and estimate system, resulting in a 25 percent increase in collection rates within just six months. According to Experian, hospitals that utilize self-service portals for personalized patient fee estimates can increase payment collection rates by up to 133 percent.
In this guide, we'll dive into the importance of transparent patient fee estimates and explore how they directly impact medical billing collection rates.
Why Accurate Payment Collection Rates Matter for Your Practice's Financial Health
Strong payment collection rates are vital to your practice's long-term financial health. The industry benchmark for patient responsibility collection rates is approximately 80 percent, but providers should aim for closer to 90 percent. However, new data shows that the average medical billing collection rate is far lower. In 2024, average rates dropped to just 34.4 percent for commercially insured patients. For hospitals and larger health systems, rates aren't much better, at below 48 percent.
Poor patient payment collection strategies and a lack of transparency cost your practice. Low collection rates contribute to higher administrative costs and an increase in bad debts. In 2023 alone, healthcare providers wrote off over $17 billion in bad debt. That significant hit in revenue affects practice operations. Administrators spend more time chasing payments. Meanwhile, squeezing margins limits the types of investments your practice can make in improving patient care and technology.
How Patient Fee Estimates Transform Your Medical Billing Collection Rate
Covering healthcare costs is a significant source of stress for patients. With per capita healthcare expenditures surpassing $16,000 in 2024, it's not difficult to see why. Upfront patient fee estimates make a difference. When patients fully understand their financial responsibilities, they're far more likely to pay on time and in full. That's because the transparency provided helps reassure patients that they won't receive any surprise bills that could suddenly impact their budgets and bottom lines.
Upfront estimates help reduce payment delays and improve your practice's cash flow. In a survey from Experian, 81 percent of respondents said that accurate estimates helped them better prepare to pay for healthcare costs. According to an MGMA financial report, practices that utilized price estimation tools experienced faster and more predictable cash flow due to improved collection rates. In a study by Health First, pricing transparency led to a 27 percent increase in upfront payments, which totaled over $2 million in annual revenue!
Proven Patient Payment Collection Strategies That Increase Revenue
Ready to improve your practice's patient responsibility collection rates? Here are a few strategies you should consider implementing.
• Offer Pre-Service Estimates: Timing is everything. To help ease a patient's worries and give ample time to budget for payments, provide accurate healthcare payment estimates before rendering any service or treatment. Upfront transparency eliminates surprises and encourages timely payments.
• Provide Upfront Payment Options: Payment flexibility matters. One health system experienced a 173 percent increase in patient responsibility payments after offering payment plans. When your practice offers payment options, patients are more likely to commit and pay consistently, reducing your practice's bad debt.
• Use Digital Payment Tools: Digital tools and self-service platforms can encourage timely payments. The right tools enable patients to make immediate payments or schedule them, reducing payment delays.
• Communicate Clearly and Proactively: Provide follow-ups and reminders. Make it easy for patients to reach out for clarification, and highlight how your practice calculated patient fee estimates. That transparency helps justify costs and helps build trust.
When you pair these patient payment collection strategies with transparent estimates, you can maximize collection rates. It's all about providing transparency and being upfront with your patients. When you let your patients know what to expect from a financial standpoint, you're setting them and your practice up for success.
Implementing Effective Healthcare Payment Estimates in Your Practice
Creating accurate patient fee estimates is easier than you may think, but it requires technical precision. When developing estimates, you must consider insurance eligibility, patient history and payer contract rates.
Begin by verifying insurance coverage and patient eligibility. Real-time insurance verification tools can do this in minutes, helping you check fine details like copays, deductibles, coverage limitations, pre-authorization requirements and more, all from a CPT code level. Next, use updated fee schedules while considering payer contract rates. Relying on fee schedules can help prevent discrepancies between what your practice expects to collect and what the patient actually owes.
Finally, review a patient's history. Doing so can help generate more precise estimates while anticipating potential variations in service needs.
Fortunately, there are many great tools available to help practices like yours generate healthcare payment estimates. Software like Fuse automates the process, performing insurance verification before using that granular benefits data to create patient cost estimates.
Whether you do things manually or let technology take over, staff training is crucial. Front desk staff should understand how your estimate process works, enabling them to communicate effectively with patients. Staff should know how to explain calculations and clarify that actual costs may differ. They should also learn how to review payment options and handle patient questions with confidence, further building trust.
Optimizing Patient Responsibility Collection Through Transparent Pricing
Patient payment responsibilities continue to grow. As mentioned earlier, per-capita healthcare spending is on the rise. However, how much individuals pay is also increasing. Since 2000, the patient portion of healthcare payments rose by 30 percent. A growing number of patients are now on a high-deductible health plan, resulting in greater out-of-pocket costs.
For healthcare providers and practices, clear communication and pricing transparency are key to strong collection rates. Your practice should present estimates early in the patient journey, prioritizing both accessibility and understanding.
The best approach is to present estimates in plain language, avoiding complex medical jargon. Highlight patient responsibilities, use visual aids and present payment options upfront. To provide additional clarification, ensure that staff are available to communicate with patients across different channels. Train staff to communicate empathetically and confidently, and consider implementing pricing estimates with digital payment tools to encourage action.
Start Improving Your Collection Rates Today with Better Fee Estimates
Improving collection rates can transform your practice, setting it up for greater financial success and stability. While many patient payment collection strategies can move the needle, offering upfront pricing estimates and greater transparency packs the biggest punch. Implementing estimate systems that prepare your patients for the financial aspects of healthcare can lead to impressive returns, with practices enjoying a 15 to 40 percent improvement in patient responsibility collection rates.
Fuse is a tech solution that automates estimation calculations, streamlining your workflow and improving estimate accuracy. Fuse dramatically reduces administrative burden while paving the way to a far better patient experience. With real-time insurance verification, automated onboarding and precise patient price estimates, you can't go wrong.
Schedule your Fuse demo today to learn more and see price estimation automation in action!
Boosting Medical Practice Revenue: The Critical Role of Patient Fee Estimates in Collection Success
Proper, error-free medical insurance verification is vital for both patients and practices. According to the latest data, about 92 percent of Americans have insurance for all or part of the year. That means a vast majority of patients coming through your practice will use their coverage to pay for at least part of their care.
An inefficient insurance verification process can be a nightmare for practices like yours, resulting in unpredictable cash flow, errors that require considerable time fixing, frequent claims denials and a host of other headaches. For patients, verification mistakes and delays can result in surprise bills that erode trust.
Insurance verification mistakes are more common than you might think.
According to a survey by Experian, 56 percent of provider respondents said that errors are a primary cause of denied claims. Those mistakes are disrupting revenue cycles and costing the industry billions of dollars annually. Practices reportedly lose up to 5 percent of net patient revenue due to errors, with some studies saying that improper healthcare insurance verification costs practices up to $25,000 per physician annually.
With errors causing delays, increased administrative burden and negative impacts to revenue cycles, more and more practices are seeking better ways to verify patient insurance. In this blog, we'll explore insurance verification best practices that make a difference, helping you handle this all-important administrative task more efficiently than ever.
Why Medical Insurance Verification is Critical for Your Practice's Success
Financially, poor medical practice insurance verification has a significant impact. As mentioned earlier, errors are a leading cause of claims denials, and the healthcare industry loses billions of dollars annually dealing with them. Larger health organizations incur losses of as much as $5 million in revenue each year due to denials and the increased administrative costs of trying to fix them. Studies suggest that the cost of reworking a single claim can cost practices anywhere from $25 to over $100. Not only that, but mistakes can delay payment by as much as 90 days, creating unpredictable cash flow for your practice.
The average practice spends more than 12 minutes manually verifying patient insurance, amounting to hours of monotonous work for a day's worth of patients. That's not considering the time it takes to chase mistakes and correct them.
Not only are there additional costs, wasted revenue and increased administrative burden, but patients suffer, too. With a majority of Americans worried about healthcare costs, surprise bills and delays caused by clunky insurance verification processes can cause patient satisfaction scores to plummet. Those issues that can then lead to low collection, retention and referral rates, ultimately affecting your practice's reputation. The consequences of inefficient processes and insurance verification mistakes are monumental, hindering your practice's path to success.
The Complete Patient Eligibility Verification Process Step-by-Step
Healthcare insurance verification workflows can vary, but a standard process will begin as soon as a patient schedules an appointment.
1. Collect Demographic and Insurance Information: When scheduling appointments with patients, collect the basics. You'll need demographics information, contact details and a photo of the patient's insurance card. Confirm policy numbers, group numbers, etc. Collecting this data as early as possible will allow you to verify patient insurance long before their appointment.
2. Confirm Policy Status and Coverage Details: Run initial checks to confirm coverage. Use payer portals to check effective dates for policy benefits, plan type, in-network status, copay, coinsurance, deductibles and more.
3. Check Treatment Eligibility: Verify coverage for planned services. Check eligibility at the CPT code level via payer phone calls. Run verification early to ensure that policies cover intended treatments. Handling this process early will give your practice ample time to contact patients if any issues arise.
4. Identify Pre-Authorizations: Remember to check for any restrictions or pre-authorization requirements. If the policy requires pre-authorization, submit requests as soon as possible. Routine approvals can take up to two weeks, with more complex procedures taking up to a month. Handle submissions early on to prevent delays.
5. Ongoing Patient Eligibility Verification: In the 48 to 72 hours before any patient's appointment, go through the medical insurance verification process again to confirm eligibility. Running an additional check before an appointment will help ensure accuracy, preventing mistakes that could result in denials. At this time, create fee estimates and confirm patient payment responsibilities.
6. Check-In Verification: During patient check-in, ensure that authorizations aren't expired, collect payment methods to prevent collection delays and communicate with patients about their responsibilities.
Advanced Verification Process Strategies That Reduce Errors
Even with a strong workflow, insurance verification mistakes can happen. Here are several strategies to mitigate the risk of errors and ensure smooth sailing for staff and patients.
• Invest in Automation Tools: Consider using verification software that can automate this process. Verification software can run checks in minutes, pulling data from payer portals. These tools can reduce staff workload and prevent the creation of redundant data. They can also flag you to potential issues that may result in claim denials.
• Integrate Tools Into Existing Systems: Integrate your tools with your EHR and practice management systems. Doing so will minimize errors caused by manual data entry while ensuring data consistency between systems.
• Combine Verification Methods: State-of-the-art insurance verification processes pair payer portal checks with phone calls. Healthcare clearinghouse platforms and your EHR's portal offer quick confirmation, but they won't provide granular benefits data. To get that, you must call payers directly. Use both methods to avoid surprises and understand eligibility at the CPT code level.
• Document Everything: Record call details, save eligibility responses in patient records or billing systems, document key benefits details and standardize file naming structures. You want strong and consistent documentation to create a clear audit trail that you can reference should issues arise later.
• Train and Cross-Train Staff: Always spend time training and cross-training your staff. Teach your team how to use tools and software solutions. Ensure everyone can perform eligibility checks to prevent dependence on a single person, and monitor performance by tracking metrics to address skills gaps that could impact your insurance verification process.
How to Verify Patient Insurance Coverage Accurately Every Time
Maintaining accuracy as you verify patient insurance coverage is about asking the right questions. Whether using a portal or calling insurers directly, always begin by confirming the patient's plan status, effective dates and in-network eligibility. Verifying these details can help prevent denied claims from the jump. From there, you can dive into more information about a patient's financial responsibilities. Inquire about copays, coinsurance and deductibles. Confirm the amounts and deductible status to help patients understand what they need to pay out of pocket.
To understand pre-authorization requirements, call payers directly. Verify coverage at the CPT code level to learn about requirements like referrals, visit limits and authorization thresholds. Here are a few targeted questions to ask:
• Is this CPT code covered by the patient's policy?
• Are there any prior authorizations or referrals required?
• Does the patient's policy have coverage limitations for this CPT code or provider type?
• What are the patient's estimated financial responsibilities for this visit?
As always, be meticulous about documenting responses. Documentation should include the date of the verification, the name of the representative you spoke with, reference numbers and any other relevant details for auditing. Record a summary of coverage benefits, including specific authorizations and patient responsibilities. Save those records in your billing system or the patient's EHR for easy reference.
Common Healthcare Insurance Verification Mistakes to Avoid
Insurance verification mistakes are common and can happen to even the most well-trained staff. Fine-tuning your process and adopting insurance verification best practices goes a long way. However, you should also train your team to avoid the following mistakes:
• Waiting Until the Last Minute: Don't wait until check-in to verify patient insurance. Verification should occur as soon as possible. Perform patient eligibility as soon as possible after setting an appointment. At the latest, aim to complete verification 48 to 72 hours before a scheduled visit.
• Missing Information: Incomplete data will create delays during the insurance verification process. Collect all relevant data, including everything on a patient's insurance card, and ensure patients complete forms in their entirety. Store that data in billing and EHR systems for easy reference.
• Incomplete Verification: Your practice needs comprehensive information about a patient's coverage and eligibility. Create a standardized verification checklist for every patient, reminding staff to collect everything from coverage details to plan status and deductibles.
• Weak Documentation: Failing to record responses and reference numbers during the verification process can result in incorrect information and a nonexistent audit trail. Standardize verification documentation and immediately log records in the EHR.
•Assuming Coverage: Don't assume that patients have coverage for a service. Always perform CPT code-level checks, especially for high-risk treatments or procedures, to understand specific limitations, authorization requirements and more.
• Using Only Payer Portals: Relying solely on payer portals will leave out critical information. You must call payers over the phone to get specific coverage details at the CPT code level.
• Ignoring Secondary Coverage: Overlooking secondary coverage may result in partial payments, unnecessary delays and collection challenges. Always ask about additional coverage and perform all necessary verifications.
Maintaining accuracy should be a top priority. Standardize your insurance verification process and create a checklist for staff to use, ensuring everyone gathers all necessary information. It's also a good idea to verify at various points, including after scheduling an appointment, several days before a patient's visit and during check-in. Doing so will allow teams to double-check information for accuracy, preventing errors that could cost your practice. Finally, perform regular audits to review efficiency and quality.
Medical Practice Verification Technology Solutions
Fortunately, you no longer have to rely on manual insurance verification processes. There are many great tech solutions available that can accelerate the process, all while saving time and minimizing the risk of errors.
Automated verification systems streamline the process by checking patient eligibility and benefits against payer databases. Real-time eligibility tools are also available, providing instant access to insurance information to confirm coverage before rendering services. Software solutions that integrate with practice management and EHR systems take things further, ensuring seamless data flow and propagation. Integration can reduce manual data entry errors and duplicate information, enhancing overall workflow efficiency.
Insurance eligibility software can revolutionize your practice's entire approach. Manual approaches are time-intensive and costly. Meanwhile, automated verification can take mere minutes and cost far less. When you consider the costs and time involved with correcting errors and dealing with claims denials, the benefits of adopting tech solutions are undeniable.
Best of all, practices of all sizes have much to gain. Smaller practices can recoup the costs of implementation within the first few months. Larger practices benefit from scalability, gaining the ability to verify insurance for a high volume of patients without additional investments in staff, resulting in a significant ROI.
Transform Your Revenue Cycle with Streamlined Insurance Verification
Improving your insurance verification process can benefit your practice in countless ways. But more importantly, it paves the way to a far better patient experience. Patients already have anxieties about paying for healthcare, with many delaying it entirely due to worries about the financial side of receiving care. When you follow insurance verification best practices and streamline your practice's approach, you can put those worries to rest. It's a way to offer transparency and peace of mind to patients, which will lead to great success for your practice.
When you want to make positive changes that benefit your patients, check out Fuse. Fuse is a healthcare software solution that can automate patient insurance verification, performing CPT code-level checks quickly and efficiently. Fuse can do the heavy lifting, improving practice operations and staff efficiency while reducing denials, facilitating faster payments and increasing patient satisfaction.
Schedule your Fuse demo and consultation today to see automated insurance verification in action and discover the many ways it can transform your practice.
Essential Best Practices for Verifying Insurance Every Medical Clinic Needs
In most practices today, you almost expect to see the same scene: A crowded waiting room full of patients with front-desk staff scrambling to enter data from a stack of clipboards. Sound familiar? An outdated patient onboarding process is a recipe for disaster. Paper forms and old-school processes lead to lengthy wait times, a high risk of data entry errors, frustrated patients and overworked staff.
Did you know that patients spend, on average, 15 to 20 minutes completing forms in a waiting room? If they're a new patient, they often spend even longer. That time adds up, putting a significant burden on your administrative staff while starting patient visits off with a frustrating experience.
It doesn't have to be that way. A streamlined digital patient intake process can address those common pain points and more, giving your practice a competitive advantage while simplifying workflows across the board. Recent surveys show that 73 percent of patients prefer digital intake options. Digital solutions make things easier for everyone, freeing up your staff to focus on delivering top-quality patient care while making visits less stressful for patients. Digital approaches also significantly reduce data entry errors that could cause chaos downstream.
Why Traditional Patient Registration Systems Are Failing Your Practice
While the pandemic certainly accelerated the adoption of digital intake processes and online patient portals, many clinics still use paper forms. One survey suggested that a significant number of practices still use paper processes, and a whopping 88 percent of hospitals rely on manual data entry for patient intake. Those outdated processes hinder medical practice in numerous ways.
• Clipboard Management: No one likes dealing with stacks of bulky clipboards. Not only do they waste valuable space, but staff must keep track of which patients have clipboards and which have already submitted forms.
• Illegible Handwriting: Hard-to-read handwriting can be a nightmare. Staff must spend time trying to decipher illegible writing and correcting inputs.
• Duplicate Data: Without automated patient registration, teams must manually input data into electronic systems or match information across records. That workflow creates a high risk of duplicate data entries. One study found that duplicate records can cost practices up to $1,000 to correct duplicated data and records.
• Manual Error: With manual data entry comes a risk of human error. Even the most vigilant administrators can make mistakes, but they can be costly. Up to 86 percent of all healthcare mistakes are administrative and a direct result of inaccurate data entry.
• Insurance Verification Delays: Errors during registration and insurance verification are reportedly the cause of 25 percent of all insurance claims denials. With incorrect information, insurance eligibility checks take longer. Practices also waste valuable time and effort in identifying errors, repeating verification checks and reworking claims forms.
• HIPAA Compliance Risks: Paper forms are more challenging to secure. They're more vulnerable to theft, misfiling and unauthorized access, presenting risks of HIPAA violations.
On top of those concerns, paper forms create a less-than-stellar patient experience. Most clinics ask patients to arrive up to 20 minutes before an appointment, all to complete paper forms. It's a frustrating process made worse by the fact that most of the information provided is redundant. In one survey, 83 percent of respondents said they had to provide duplicate information.
These issues all compound to affect your practice's bottom line. A poor patient experience actively harms your reputation. Furthermore, outdated processes that are prone to human errors can negatively impact collection rates, delay reimbursements and create additional administrative work, ultimately leading to staff burnout.
The Complete Digital Patient Intake Journey: From First Contact to Treatment
In 2025 and beyond, patients expect a seamless digital experience. Patient experience optimization should be a top priority, but what does a patient's digital journey look like? The ideal patient experience begins before their visit, featuring online support and automated patient registration.
• Online Appointment Booking: Patients should be able to schedule appointments digitally without having to call your office. A reported 67 percent of patients prefer online booking. Allowing people to choose a date and time that works for them can help reduce no-shows. Send automated reminders to prevent last-minute cancellations.
• Pre-Visit Patient Intake Software: Why spend time in the office completing forms when you can streamline patient intake by having them do it at home? With patient intake software, your practice can encourage individuals to complete intake forms, consent documents, medical history forms and more before their visit. Digital healthcare intake management and patient registration systems save valuable time and can reduce errors associated with manual data entry.
• Insurance Verification: Real-time insurance verification ensures that your practice and your patients understand coverage before a visit. Patients will have a better understanding of their insurance eligibility, and practices like yours can address any issues before rendering treatment or submitting claims.
• Cost Estimates: In addition to verifying insurance, your practice can provide automated digital cost estimates. Doing so gives patients a better understanding of their financial responsibilities. It reduces anxiety over clinic visits, helps them prepare for visits and can help increase collection rates.
• Visit Check-In Upon arrival, self-serve kiosks or tablets allow patients to check in quickly and effectively. Digital systems save time, eliminate the need for traditional paperwork and prevent lengthy wait times.
Essential Features Your Intake Software Must Have
Patient intake software can transform your practice, improving healthcare intake management strategies while saving everyone time and effort. The best software will streamline workflows and help improve your revenue cycles. There are many features to look for, but the following are non-negotiables your software needs to have.
• HIPAA Compliance: HIPAA compliance should be standard. The software you use should protect all digital intake forms, safeguarding protected health information (PHI) to meet federal regulations. Look for features like strong encryption and user authorization.
• Smooth EHR Integration: You want your patient onboarding process to be as smooth and error-free as possible. That requires smooth EHR integration. Integration with existing EHRs ensures that data flows between systems without a hitch, preventing duplicate data and errors.
• Mobile Optimization: An estimated 55 percent of patients in the U.S. prefer using mobile devices for managing healthcare appointments and records. Patients should have the ability to complete digital intake forms on smartphones or tablets.
• User-Friendly Interfaces: Intuitive interfaces and guided workflows benefit both staff and patients. Clunky experiences only add frustration, impacting abandonment rates and creating more incomplete forms your staff needs to fix.
• Customizable Forms: Digital patient intake software should allow you to create and customize forms to meet your practice's needs. That includes customizing forms based on your specialty and branding.
• Insurance Verification Capabilities: Real-time insurance verification features check eligibility in minutes, eliminating manual work and delays while reducing the risk of errors. Completing verification processes before a patient's visit will save time and ensure timely care.
• E-Signature Support: Software needs to support e-signatures. Without it, you'll still rely on paper forms. E-signatures can streamline consent processes.
• Photo Capabilities: Photo capture features can enhance patient records and help staff verify identities.
•Technical Considerations: All software that helps improve healthcare intake management needs strong security protocols, including robust encryption and access control. However, it's also wise to seek solutions with API capabilities. APIs help with scalability and integration.
HIPAA-Compliant Digital Intake Forms That Patients Actually Complete
It's one thing to make intake forms available digitally. However, it's another to design forms that patients will actually complete. There's an art to developing intuitive, easy-to-understand digital intake forms. Failing to consider the patient experience when completing these forms can result in high abandonment rates and even more frustration.
First, ensure that forms are accessible on the devices that patients want to use. Take a mobile-first approach. Ensure that all forms are optimized for mobile devices and support features like touch input. Because mobile screens are comparatively small, keep scrolling to a minimum and ensure that all buttons and text are large enough for optimal visibility.
Forms themselves need to be concise and logically organized. The best approach is to use progressive disclosure. Only show questions that are relevant to patients in the moment. For example, you don't need to ask patients questions about insurance if they plan to pay out of pocket. Therefore, you'd only unveil insurance-based questions once patients answer "yes" to a question like "Do you have insurance?"
Questions should make sense and flow from one to the other. Generally, it's best to ask for personal details before moving on to insurance, medical histories and consent. To make things more predictable, implement a visual progress bar.
When completing more complex forms, the key is to simplify the process. Throwing tons of confusing questions at patients will only increase abandonment rates. You want to break things down into manageable chunks. Provide clear queries and guidance. Your digital intake forms can also offer inline tips to help patients understand what you're asking. Intuitively guide patients from one section to the next until they reach completion.
Thoughtful UX design goes a long way. Put yourself in your patients' shoes and see how it feels to complete forms yourself. Fine-tune design elements and simplify things as much as possible. When done right, the process will be a cinch.
Automated Patient Registration Features That Save Hours Daily
If you're looking to streamline patient intake as much as possible, automation is the way to go. Fortunately, patient intake software can have automated features that make the lives of your staff and patients significantly easier. Here are a few to look for.
• Insurance Verification and Eligibility Checks: Automated insurance and eligibility checks can save hours of manual work. You can verify insurance coverage in real-time. Software that performs checks on the CPT code level can even provide more information bout preauthorization requirements, limits and other coverage specifics. Manual insurance verification takes, on average, 12 minutes per patient, assuming you don't need to make a phone call to a payer. However, with automated real-time verification, you can do it in just a few minutes.
• Demographic Updates: Automated software helps practices ensure accurate and updated patient information. Integration with practice management systems and EHRs can streamline demographic information capture, preventing duplications and errors.
• Appointment Confirmations: Systems that send out automatic reminders and confirmations can dramatically reduce the rate of cancellations and no-shows. Furthermore, you free up your staff to focus more on patient-centered care rather than spending hours on the phone.
Overall, automated features can have a positive ripple effect on your practice and its revenue cycle. These features virtually eliminate the need for hours of manual data entry. Additionally, they help reduce errors that often require hours to correct. With seamless integration with existing practice management systems, automated tools can reduce administrative workload by as much as 30 percent. According to the 2024 CAQH Index, automated workflows have the potential to save the entire healthcare industry around $20 billion.
Healthcare Intake Management Systems That Scale With Your Practice
As practices expand, healthcare intake management systems must grow, too. Scalability is something your practice needs to consider when choosing the right digital solutions and tools. It's essential to maintain operational efficiency while striving for long-term success.
Some key features and scalable capabilities to consider include multi-site support, customized options tailored to different specialties and robust analytics.
Multi-site support offers centralized management capabilities, enabling administrators to deliver consistent experiences across multiple locations. Having the ability to manage several locations can reduce administrative work while maintaining compliance and high standards across the board.
Customized options ensure your software can accommodate the unique needs of different specialties. Scalable solutions will offer custom frameworks, workflows and consent forms tailored to each specialty.
Finally, strong reporting capabilities and analytics help practices gain actionable insights when it matters. Easy-to-read dashboards, comprehensive reports and trackable KPIs make it easy to identify opportunities for improvement on your journey to growth and enhanced efficiency.
Growing your practice can be overwhelming, and there are many scalability concerns to address. To choose the right software for your needs, turn to options that offer enterprise-level features. API integrations, advanced user permissions and authorizations, clear audit trails and in-depth reporting give you all the tools to grow. Additionally, these features can help create a roadmap for sustainable expansion, paving the way for growth without the associated growing pains.
How to Streamline Patient Intake Without Overwhelming Your Staff
Making the switch to more efficient patient registration systems can be overwhelming for your staff. There are many benefits on the horizon, but you can only reap those rewards if you can manage the transition without issue.
Start by communicating with your staff. You want to explain how the change can benefit your team, highlighting how automation will support roles while streamlining workflows. Gather feedback early and listen to your staff. Being receptive and transparent can increase buy-in.
From there, you should map out existing intake processes. Identify the pain points your staff encounters and see how new solutions and tools can alleviate them. Demonstrate those improvements to your team to emphasize further the positive impact this transition can have.
Like any other major workplace change, it's best to implement new solutions in phases. For example, you can begin by allowing patients to schedule appointments online. Then, you can move towards making forms available for patients to complete before their visit. Once you have successfully implemented those changes, you can move on to automated real-time insurance verification and more complex tasks. Take things slow, allow staff to familiarize themselves with their new workflows and continually accept feedback.
It's also wise to still make paper forms available during the early stages of your transition. Doing so will accommodate patients who prefer them and can ease the transition to digital workflows for your staff.
As always, provide hands-on training and support. Change can be difficult for staff members who are accustomed to doing things one way, even if those old methods are less efficient. Provide guidance when necessary, resolve issues promptly and make support easily accessible to all.
Measuring Success: ROI Metrics That Prove Your Investment in Digital Intake
Investing in tools that offer automated patient registration and streamline intake processes is a significant move. However, it's an investment that can pay off. To prove the value of new initiatives and tech implementation, you need to track several KPIs.
Practices can present these metrics in executive summaries and ROI reports to prove the efficiency of patient intake software. Furthermore, tracking the right KPIs can help you optimize your strategies. Using dashboards to track key metrics makes identifying opportunities for improvement easier than ever, leading to enhanced medical practice efficiency and patient experience optimization that you can quantify.
Core KPIs you should monitor include:
• Wait Times: Reduced wait times can show real value in the tools you use to improve the patient registration process. Currently, the average wait time for patients is 20 minutes. However, digital intake forms and automation can cut that in
• Patient Satisfaction Scores: Patient satisfaction scores can easily highlight the impact of tech investments. Roughly 73 percent of patients prefer digital intake processes, significantly improving patient satisfaction from the start.
• Staff Overtime: Substantial administrative burden caused by outdated manual processes can lead to hours of staff overtime. Tracking this metric will highlight how much patient intake software reduces workload.
• Revenue Cycles: Faster revenue cycles are always a plus. Because digital intake software and automation save time while reducing errors, you can track this metric to show how changes help your practice beat the industry benchmark of 30 to 50 days in accounts receivable.
• No-Show Rates: The average no-show rate is between 5 and 7 percent, but some specialty clinics can experience rates as high as 30 percent. With online appointment-setting and automated reminders, the right software can help you see marked improvements in this area.
Ready to Transform Your Patient Experience?
The patient experience begins long before a visit to your clinic. Practices that prioritize highly efficient digital patient intake processes gain a significant advantage. Modern patients expect digital convenience and mobile-friendly interactions. Adopting patient intake software early on to meet the demands and expectations of patients can give your practice a competitive edge, positioning it as a forward-facing practice that focuses on creating a stellar experience for patients.
With more and more practices leveraging technology to streamline patient intake and other administrative workflows, you can't afford to hold back. Fortunately, Fuse is here to help you leverage automation to save time and maximize revenue.
Fuse is a state-of-the-art software solution that automates patient intake, CPT code-level insurance verification and cost estimates. With Fuse, you can transform your practice in numerous ways and achieve a rapid return on your investment. With implementation support and more revolutionary features to come, you have nothing to lose and everything to gain.
Schedule your Fuse demo today to see firsthand how it can help you create that five-star experience patients want.
How to Create a 5-Star Digital Patient Intake Experience That Transforms Your Practice
These days, patients no longer leave their healthcare to chance or rely on basic referrals to find the care they need. Today's patients set the agenda, conducting more research about practices and providers than ever before in history. Their tool of choice? The Internet!
In 2023, approximately 5 percent of Google's daily search volume was health-related, a figure that's likely higher today. Recent surveys suggest that a vast majority of patients (roughly 77 percent) research online before booking appointments. One study found that over 90 percent of patients read provider bios and gather information about a practice before reaching out through official channels. That data highlights a significant shift in patient behaviors. People take an active role in finding the best care possible. To boost patient acquisition, your medical practice marketing needs to keep up.
Search engine optimization (SEO) is a digital marketing strategy that can lead to long-term growth and success for practices like yours. Strong SEO for medical practices can establish your website as a trusted authority, attracting potential patients and growing organic search traffic. Shifting focus toward SEO can make a difference. Estimates say that more than half of all visits to healthcare websites come from organic searches. While results can vary, numerous case studies demonstrate that effective SEO practices pack a punch. One case study showed that for every $1 spent on SEO, practices can net between $4 and $10 in revenue. In another case study, a practice increased organic search traffic by over 46 percent, resulting in a 16 percent increase in year-over-year appointment requests.
There's more than enough evidence to demonstrate that SEO is effective across various industries, including healthcare. However, medical practices have many unique challenges that other types of businesses don't. Numerous regulations impact how practices can advertise their services. There's a delicate balance between maintaining HIPAA compliance and meeting E-E-A-T requirements needed to maximize online visibility. In this guide, we'll explore the importance of SEO for medical practices and provide game-changing strategies that can help you attract more patients while setting your practice up for long-term growth.
Why Healthcare SEO Optimization Drives More Patient Conversions
Search engine optimization is all about building a strong, authoritative online presence. This strategy involves optimizing your website for search engines, making it appear as high as possible on search engine result pages (SERPs). It aligns with modern patient behaviors, presenting your practice as the best choice for their needs, while also providing relevant information that goes into their decision-making.
There are many reasons why healthcare SEO optimization is so effective. However, it all revolves around trust. When patients are looking for providers and practices, several key factors influence their decision-making process, and medical practice SEO can have a bigger impact than you may realize.
• Higher Rankings: Did you know that over 75 percent of people never go beyond Google's first page of results? Most people trust search engine algorithms to deliver high-quality results. Therefore, having your practice's page appear high up on the first page automatically signals reliability.
• Reviews Positive reviews matter. Not only do most patients read them before booking an appointment, but reviews can also influence rankings. Practices with high online visibility and positive ratings are more likely to convert searchers into patients.
• Website Professionalism: SEO ranking factors like mobile optimization, website speed and UX design help put the best websites at the top of a results page. Part of medical practice SEO is having a modern, easily accessible website that patients will enjoy visiting. In addition to helping you rank higher, a well-built and optimized website will reflect positively on your practice. It signals professionalism, another major trust factor that can influence patient choices.
• Authoritative Content: SEO for medical practices involves more than just using keywords throughout your content. Your strategy should emphasize high-quality content that establishes experience, expertise, authoritativeness and trustworthiness (E-E-A-T). Publishing content that meets E-E-A-T guidelines will lead to improved rankings. More importantly, it helps build trust among potential patients.
• Local SEO: Because most patients are looking for local healthcare providers, prioritizing local SEO for doctors and practices can lead to measurable improvements. Searches containing "near me" have reportedly increased by over 500 percent in the last few years, primarily driven by the widespread use of mobile devices. One study found that 42 percent of people making local searches click on one of the results that appear on a Google Map Pack, highlighting the importance of local SEO and complete business profiles.
The ROI Benefits of Healthcare SEO Optimization
When you compare the costs of a robust SEO strategy to more traditional medical practice marketing techniques, SEO can provide a much better return on your investment. The average cost per patient acquisition can vary significantly depending on your market and level of competition. However, the average medical practice spends about $300 on SEO to acquire a new patient.
That's significantly less than what practices spend on other marketing channels. Specialty practices can expect to pay around $800 to acquire a single new patient through PPC ads on Google. Meanwhile, practices offering elective or cosmetic procedures can spend up to $1,500. Providers that incorporate television or radio ads can find themselves paying thousands to convert a single patient.
SEO is more cost-effective every way you look at it. But that's not all. The ROI for healthcare SEO optimization compounds, continually improving over time. Unlike paid ads, traffic doesn't disappear when spending stops. Your SEO efforts continue to pay off over time, making it easier to experience gradual growth while competing with larger systems that have bigger marketing budgets than your own.
Essential SEO for Medical Practices: Foundation Elements
Successful medical website optimization starts with a strong foundation. It can feel overwhelming, especially when up against larger healthcare systems with seemingly bottomless marketing budgets. However, the beauty of SEO is that it's accessible to practices of all sizes. What's important is that you take the time to get things right and set your site up for success.
SEO takes time. While paid ads and more conventional strategies can provide a temporary boost, strong medical SEO strategies are about the long game, building organic traffic that leads to continued success and visibility. We'll get into the importance of local SEO and high-quality content soon. However, for now, let's cover the basics.
• Speed Improvements: Ever try to use a website that was sluggish and slow to load? No one enjoys that, and search engines don't view poor performance favorably when developing rankings. Aim for a load time of less than three seconds by utilizing browser caching or a CDN. You can also prioritize over-the-fold content loading, compress images and more.
•Mobile Optimization: The latest estimates show that roughly 68 percent of all health searches occur on a mobile device. Mobile medical website optimization is a must. Search engines like Google use mobile-first indexing. Therefore, sites not optimized for mobile devices rank lower than those that are. You want to ensure your website is accessible on the go.
• Security: Search engines like Google prioritize secure websites using HTTPS. Successful healthcare SEO optimization requires that all pages utilize SSL to build trust and ensure patient information remains safe.
• UX Enhancements: A positive user experience can make a website stand out. Search engines rank websites based on their usefulness and relevance. When developing a medical practice SEO strategy, consider revamping your website to ensure easy, enjoyable navigation. Utilize menus for navigation, provide easy access to appointment booking forms and make all pages easy to find.
• Descriptive Tags and Descriptions: On-page SEO elements like title tags and meta descriptions matter. They help search engines understand your site and can influence a user's decision to click your link. Incorporate relevant keywords and location data to improve your healthcare digital marketing content.
• Schema Markup Implementation: Like tags and descriptions, schema markups help search engines understand what your website is all about. The right structured data on each page can lead to improved search result visibility.
• Internal Linking: Don't forget to link to other pages on your website. Internal linking can significantly improve site navigation and strengthen topical authority. It can also increase the amount of time visitors spend on your site, increasing the chances of conversion.
• AI-Ready Content Structure: Format content with clear headings, FAQ sections, and structured data markup. As AI-powered search grows, well-organized content that answers specific questions will be more likely to appear in AI responses and voice search results.
E-E-A-T Requirements for Medical Content
E-E-A-T is an acronym that reflects what Google's human quality raters consider when evaluating the credibility of online content. As mentioned earlier, E-E-A-T stands for experience, expertise, authoritativeness and trustworthiness. The specifics of the algorithm that Google uses to find and rank relevant websites are a mystery, and they frequently change to align with user needs. However, following E-E-A-T requirements is an excellent way to ensure you're creating content that search engines find favorable.
Embracing E-E-A-T is vital for all forms of digital marketing. However, things are different when implementing medical SEO strategies. Medical content falls under the "Your Money or Your Life" (YMYL) umbrella. YMYL is a collection of topics that Google applies higher standards to, as they could significantly impact a person's health, safety, happiness or financial stability.
When developing content, it is essential to keep E-E-A-T in mind. However, to ensure Google elevates your content instead of suppressing it to protect users from harm, you need to provide proof of E-E-A-T. To meet all E-E-A-T requirements for medical content, it needs to meet the following criteria:
• Content must be written or reviewed by qualified healthcare professionals to prove expertise.
• Content must be factually correct and backed by medical sources to build authority.
Websites and content must have transparent information about credentials, contact information and compliance to earn trust.
Medical Practice Marketing Through Local SEO Dominance
In medical practice marketing, local SEO is often more important than broader global SEO. Medical practices like yours serve people within your geographical area. While becoming an authority in your specialty on a worldwide scale is always beneficial, you want to focus your digital marketing resources toward local SEO dominance.
The first step is to complete your Google Business Profile (GBP). This free profile is often the first thing potential patients see about your practice. Optimizing it can significantly boost local search visibility.
Create a profile or claim an existing one for your business. Then, fill out every available section. Create an engaging description, provide information about your services, add photos and more, all while complying with those E-E-A-T requirements for medical content.
Once you complete your profile, you can work to earn citations and reviews to build your authority. It's also important to respond to any reviews you receive on Google. Remember: Most patients read reviews about healthcare providers and practices before booking an appointment. Negative reviews happen to every practice. What's critical is that you respond to them in a professional manner.
Respond to any reviews within 48 hours to show attentiveness. If the review is negative, acknowledge the reviewer's pain points, apologize for their experience and invite them to reach out to your practice to resolve the situation. When responding to negative or positive reviews, ensure your responses are HIPAA-compliant. For example, you should avoid confirming that the reviewer is a patient or responding with any potentially sensitive information.
Keep responses general and professional. Never respond with negativity, excuses or accusations! Always remember that people reading those reviews may become future patients. Keep your cool and remain cordial. After interacting with patients in your office, invite them to leave a Google review. Doing so can help you build up a positive reputation, ultimately benefiting your SEO efforts, while offsetting those occasional negative reviews you might receive.
Medical SEO Strategies for Google Business Profile
There are numerous ways that practices can optimize their Google profiles. Here are a few tips that can make all the difference in local search visibility.
• Complete Every Available Section: Don't leave any section blank. A complete profile is better for rankings. Include office hours, phone numbers, physical addresses, etc. You also want to provide a practice description that contains high-value keywords.
• Ensure Consistency: Triple-check that all names, addresses and phone numbers are consistent between your website, business profile and social media. Pay close attention to spelling and capitalization.
•List Available Services: List as many services as you can to cover all potential keywords patients may use to find your practice. Use descriptions that match the language patients would use. Not only does that improve understanding, but it will also signal relevance during the rankings process.
• Choose the Correct Categories: Search engines will consider the category you select when ranking your practice. The primary category should reflect your main specialty. Meanwhile, secondary categories can encompass any sub-services relevant to your practice.
• Use High-Quality Photos: Publishing high-resolution photos goes a long way in healthcare digital marketing. Ensure that you include exterior shots that patients can use to identify your building, interior shots to establish trust and photos of your staff to enhance credibility.
• Create Virtual Tours: Consider creating virtual tours that showcase your property. Many patients find visiting a new practice daunting, and a virtual tour is a fantastic way to ease their worries. Additionally, tours can enhance user engagement and establish credibility.
• Enable Online Booking: Enable or promote online booking. Google's "Reserve with Google" feature connects with third-party scheduling software, allowing patients to request appointments directly on your profile. Online booking reduces conversion friction, potentially leading to an increase in appointment bookings.
• Add FAQs: Add a FAQs section to your GBP to address common patient questions and concerns. You can also use this FAQs section to incorporate more relevant keywords.
• Post Updates Regularly: Regular posting signals to Google that your profile is active and well-maintained. Use Google posts to keep patients engaged. Provide health tips, make posts about your practice's day-to-day and more. As always, maintain HIPAA compliance while applying all E-E-A-T requirements.
Local SEO for Doctors: Directory and Citation Management
It's not enough to complete a profile and hope for the best. Successful SEO for doctors also involves getting on as many directories as possible. You want others to mention and link to your practice. Citations help to build authority. The more websites that point visitors to your Google business profile and website, the more authoritative you become.
Citations also boost local pack rankings, drive referral traffic and strengthen overall patient trust.
Work to get your practice included in local and regional directories, including those maintained by your local chamber of commerce or state associations. Doing so will validate your local presence.
To strengthen your medical practice SEO efforts, you must also get your business on medical directories such as:
• Zocdoc
• Healthgrades
• Vitals
• WebMD
• RateMDs
• CareDash
• Doximity
Focus on directories that align with your specialty. For example, mental health practices will want to receive citations from GoodTherapy, Psychology Today and Alma. Meanwhile, dental clinics should have citations from the American Dental Association and DentalPlans.com.
Consider creating a master sheet for all citations to ensure consistency and accuracy. Consistency is paramount. In addition to ensuring that all names, numbers and addresses are the same, you should use matching language when describing specialties and credentials. Having a master sheet makes it that much easier. You can also utilize third-party tools that check consistency across directories. These tools can even check for missing links and help you make updates if information changes.
Healthcare Digital Marketing: Content That Converts Patients
Now, let's talk content. High-quality content is at the heart of medical practice SEO. The entire goal is to publish content that potential patients find helpful. The more valuable and authoritative your content is, the more it'll help drive organic traffic to your website.
Focus on evergreen content that's relevant to patient concerns. All content must be HIPAA-compliant to protect sensitive information. However, it must also be informative yet accessible.
One of the most challenging aspects of medical practice marketing is striking a balance between showcasing your practice's expertise and presenting information in a way that's easy for patients to understand. Most patients aren't well-versed in medical jargon. They're searching the web to learn more about the services you provide, so you must approach content creation from a patient's point of view. That means delivering content in a format that's easy to follow, information-rich and authoritative
Medical Website Optimization for Patient Education
The best way to approach healthcare SEO optimization from a content creation standpoint is to educate. Your website's content is not intended for other healthcare providers or trade organizations. It's for the everyday person concerned with their healthcare journey. Fortunately, many types of content can resonate with patients. Here's a quick breakdown of what you can publish on your site to build authority, earn trust and convert visitors.
• Condition and Symptom Guides: Google reportedly receives 70,000 health-related searches a minute, and many revolve around specific symptoms and conditions. Symptom guides offer incredible value, providing answers and information on subjects that patients are actively seeking.
• Educational Blogs: Educational topics are another heavy hitter. As a medical practice, you can utilize your expertise to provide helpful tips or "what to expect" guides on various conditions, treatments and other relevant topics.
• Treatment Comparison Pages: Healthcare providers can address health concerns in many ways, and many patients want to learn more about their options. Content that explores the differences and similarities of treatments offers exceptional value.
• Procedure Pages: Many patients conduct research before a scheduled procedure. As part of your medical practice SEO efforts, you can create pages dedicated to detailing how the procedures your practice performs work.
• How-To Guides: How-to guides are an excellent way to earn trust. You can publish guides on how to manage conditions, prepare for treatment and handle post-procedure follow-up care, among other topics.
• Patient Stories: Patient stories and testimonials provide social proof about your practice's capabilities. They're also a great way to demonstrate how your practice approaches things differently from competitors, such as larger health systems.
When creating this content, always consider what patients are looking for and take steps to link to other pages on your site. Adding sections that cover frequently asked questions or "what to expect" goes a long way in building trust and authority while proving your expertise. Content that directly addresses a visitor's concerns can help you attract new patients while enhancing your site's search engine rankings.
HIPAA-Compliant SEO Content Creation
Search engines like Google scrutinize medical content, and for good reason. There are many legal repercussions for violating HIPAA or spreading misinformation.
Always maintain HIPAA compliance. Don't include any patient-identifiable information. Avoid using full names or detailed medical histories in your content. Instead, keep your content more generalized. The best approach is to provide general condition information without referring to specific people.
If discussing real-world cases, anonymize the data to protect your patients and practice. When gathering testimonials to publish, get explicit consent from your patients and ensure statements don't include any protected information.
Beyond HIPAA compliance, there are also several legal implications to consider. SEO for medical practices can easily fall into risky territory. Avoid making any strong claims, promises or guarantees. For example, guaranteeing positive outcomes or claiming to be the "best" provider in the area could constitute false advertising. Steer clear of any unsubstantiated claims or overstated income.
To maintain the factual accuracy of your website, always clearly identify the author's credentials and provide links to authoritative, peer-reviewed studies. It's also wise to include disclaimers where appropriate. Your content is intended solely for informational and marketing purposes. Therefore, you can't provide medical advice. Providing a disclaimer that says as such will protect your practice from liability.
Advanced Medical Practice SEO: Technical Optimization
The quality of your content matters when developing strategies for high-impact medical practice marketing and SEO enhancements. However, success hinges on more than just the content you produce. Beyond on-page SEO, you must also invest in technical SEO.
We already covered some pivotal technical details that could improve your website. These include optimizing your website's loading speed, enhancing security and ensuring your site is accessible on mobile devices. Technical SEO can influence your rankings. Search engines like Google won't rank clunky websites with poor performance. Therefore, investing in improvements to ensure your site offers a smooth experience for visitors goes a long way.
If your website also offers online booking features, ensure you get an appropriate SSL certificate. An encryption security protocol will protect patient information.
Transform Your Medical Practice with Professional SEO Implementation
Medical practice SEO isn't something you can afford to ignore. Modern patients are more involved in their healthcare than ever before, taking an active role in finding providers that meet their distinct needs and preferences. Thanks to the Internet, patients can receive care on their own terms. As a medical practice, your success hinges on your ability to reach patients where they are. Healthcare SEO optimization helps you achieve this, but it can be a significant undertaking.
Medical SEO strategies are complex, and expertise matters. Successful SEO for medical practices can pave the way to stronger online visibility, more appointment bookings and sustained growth. It provides a greater ROI than traditional medical practice marketing techniques and can even provide your practice with a competitive advantage over larger health systems with bigger advertising budgets. But to realize those benefits and more, you need professional medical website optimization and expert medical practice SEO implementation.
Put your practice on a path to success while saving time, maximizing your ROI and achieving measurable, sustainable growth that counts. Give your practice what it needs to compete with the big dogs. Reach out to Fuse today to schedule your medical practice SEO consultation and see firsthand how the right strategies can help you book more patients and boost your bottom line.
Preparing for AI-Powered Search: Future-Proofing Your Medical Practice
As AI-powered search tools become more common, forward-thinking medical practices are starting to optimize for these new technologies. While traditional SEO remains the foundation, preparing for AI search can give your practice an early advantage.
AI assistants and tools like ChatGPT are increasingly used for health-related questions, and Google's AI Overviews now appear for many medical searches. To optimize for these platforms, focus on creating content that AI can easily understand and cite. Use clear, structured formatting with descriptive headings and bullet points. Implement FAQ schema markup to help AI assistants find and present your information accurately.
The key is making your content conversational and comprehensive. When patients ask AI tools questions about symptoms or treatments, you want your practice's information to be the source that gets referenced. This means writing in natural language that matches how people actually speak and ask questions, not just how they type into search engines.
Medical Practice Marketing: The Benefits of SEO for Healthcare Providers
According to the Medical Group Management Association (MGMA), about 58 percent of medical group leaders review payer contracts annually. While more than half is great, the number of practices that then proceed to contact payers and initiate negotiations is far fewer. If your practice falls into that category, you're leaving money on the table.
The truth is that most providers aren't reaching their full revenue potential, and it's a costly mistake that many can't afford to keep making. Administrative costs are at an all-time high, with some estimates showing that the U.S. spends a whopping $1.1 trillion annually on these tasks alone. Practices spend considerable resources, yet lose up to 11 percent of their net annual revenue due to insurance underpayments and even more from unfair contract rates.
All these issues compound, placing significant financial strain on practices nationwide. About 90 percent of medical practices reported higher operating costs in 2025 compared to 2024, with expenses quickly outpacing revenue growth. The Healthcare Financial Management Association (HFMA) estimates that hospitals and health systems need to negotiate a 5 to 8 percent increase each year to break even by 2027.
Strategic contract negotiations can make a significant difference for medical practices like yours. With the right approach, you can negotiate better insurance contract terms, boosting your practice's revenue by 15 to 25 percent, all without adding new patients. In this guide, we'll explore several proven strategies that can help you secure higher insurance reimbursement rates that will maximize revenue and put your practice on the path toward financial success and stability.
Essential Steps for Successful Insurance Contract Negotiation
Negotiating higher insurance payments can be overwhelming, and it's not a quick process. Payers typically hold the upper hand due to their significant market power and financial leverage, especially when compared to individual practices or smaller group practices. However, that doesn't mean payer contract optimization isn't possible. There are many ways to negotiate better terms that benefit your practice and its bottom line.
Before initiating negotiations, it is essential to understand the process, conduct thorough due diligence and develop a strategy that positions your practice for success. Here's what a typical negotiation process entails for medical practices.
• Identify Negotiation Targets: The first thing to do is identify your negotiation target. Audit current contracts and analyze your practice's payer mix. Depending on your practice's specialty, you may have well over 25 different payer contracts. To optimize this process, you must determine which insurers cover the most significant percentage of your patient base. Payer contract optimization is all about focusing your efforts on the insurers that contribute the most to your annual revenue. Use your audit findings to identify which payers account for the majority of your revenue and those that pay below market rates.
• Identify Revenue Drivers: Next, you must identify where most of your practice's revenue comes from. You don't want to waste energy, resources or leverage to get better insurance reimbursement rates across the board. Instead, set your sights on the CPT codes that move the needle most for your practice. Follow the 80/20 rule. Typically, about 80 percent of a practice's revenue comes from just 20 percent of CPT codes used to bill payers. Use that rule to understand what rates should be up for negotiations.
• Data Collection: Don't expect to get better insurance contract terms without supplying concrete data. Before proceeding with any negotiations, you must collect data about current reimbursement rates, payment deadlines, increase clauses and more. Understand your current contract. Then, collect data about your practice. Know your numbers and prepare to present information about current overhead and operating costs. This information can help you build a case when negotiating with payers.
• Conduct Market Rate Analysis: Of course, you can't build a case if you don't understand how your current insurance contract terms compare to what's normal for the market. Know where your current reimbursement rates stand in relation to market norms. There are many ways to competitively position your practice, but proving that your rates are below market goes a long way. Perform comprehensive market rate analysis. Many resources are available. Take advantage of price transparency data, now available as part of a CMS mandate, MGMA data, information from state medical organizations and more to learn where your rates currently stand.
• Build a Value Proposition: The most significant challenge when negotiating medical provider contracts with payers is building a case as to why your practice deserves better. The information you uncover during market rate analysis makes a difference. However, you also need to develop a value proposition. Use data to show how your practice provides value to a payer's members. We'll get into the specifics of building your case soon, but it's essential to understand that this step in the process focuses solely on what your practice has to offer patients. It's about showing payers why your practice deserves more favorable insurance reimbursement rates.
• Initiate Negotiations: Once you complete your due diligence and preparations, you can initiate negotiations. However, there are timing considerations. Review the current contract terms and renewal dates to determine the best time to start negotiations. Learn about any increase clauses or auto-renewal dates. Negotiations take time, and it's typically best to start negotiating better terms roughly three to six months before contract renewal, if not sooner.
• Back-and-Forth Discussions: Negotiations are rarely one-and-done. Expect a back-and-forth with payers. Set realistic targets and consider broadening the scope of your negotiations. In addition to fighting to increase reimbursement rates, you can negotiate other terms. For example, discussing faster payment cycles, improved claims appeal processes and other specifics within payer contracts can lead to better outcomes for your practice.
• Execution and Follow-Through: After signing new insurance contract terms, monitor reimbursements and look out for underpayments to ensure payers are holding up their end of your new agreement.
Payer Contract Optimization: Building Your Foundation
Building a strong case before you negotiate insurance contract rates can make all the difference. While healthcare providers spend their days helping patients, insurance is ultimately all about business. Payers will fight to keep rates low, so it's up to practices to take the initiative, do their homework and create a rock-solid argument as to why payer contracts need review and change.
To achieve this, you must start with a solid foundation. Payer contracts are legally binding agreements that outline how a health insurance company will reimburse a healthcare provider for services provided to its policyholders. It sounds simple enough, but there are many different types of payer contracts and countless terms to understand.
Before negotiations, take the time to audit your current contracts. You want to review all terms and fee schedules. More importantly, you must collect data about your practice and market standards to understand how your current contract affects your business.
Comparing Fee Schedules and Actual Payments
When reviewing contracts with each payer your practice works with, analyze the agreed-upon fee schedules and actual payments made to your practice. Fee schedules reflect insurance reimbursement rates for specific CPT codes. Most practices follow a traditional fee-for-service (FFS) model where insurance companies pay a set fee each time a practice provides a particular service. However, that doesn't mean your practice always receives the amount covered in the fee schedule.
Actual remittances after claims processing are often lower. As mentioned earlier, underpayment is common, and practices can lose up to 11 percent of annual revenue to insurance underpayment if not caught. Underpayment can occur for many reasons, including downcoding, processing errors or unfavorable bundle rules. Whatever the case, you want to understand how underpayment affects your practice and use that information to build your case.
When auditing your contract, pull the top CPT codes and compare the contracted fee schedule to payments received by the payer. You'll likely find discrepancies. Flag them and collect all relevant data to prove your case during negotiations.
Identifying Weak Clauses
Insurance contract terms can significantly impact revenue in various ways. It's not just about fee schedules and CPT codes. Weak or risky clauses in your contract could also hurt your practice. Successful payer contract optimization involves identifying and addressing key clauses during the negotiation process.
There are many red flags to look for when reviewing contracts. Some of the biggest include:
• Strict Prior Authorization Requirements: Excessive limitations and rules about prior authorizations can severely limit revenue. Furthermore, it can disrupt and delay patient care, ultimately impacting a practice's ability to provide high-quality service.
• Unilateral Amendment Clauses: Some contracts have clauses that allow insurance companies to change terms without consulting a practice, which can be a nightmare for providers.
• Auto-Renewal Clauses: Many contracts have auto-renewal clauses, which can lock practices into outdated rates.
• Termination Clauses: If a contract has clauses that allow insurers to drop practices without cause, practices will have less leverage during negotiations.
•Unclear Payment Timelines: Contracts should have clear timelines that dictate how quickly payers process and remit payments to practices. If they don't, practices will have unpredictable revenue.
• No Escalation Terms: Some payer contracts lack escalation terms that increase rates annually. Thus, rates can quickly fall behind inflation and rising operating costs.
Understanding Non-Rate Insurance Contract Terms
Additional insurance contract terms can negatively impact revenue, resulting in underpayments, increased losses and unnecessary complexity. Familiarize yourself with existing downcoding policies, bundling rules and dispute resolution processes. Collect data to understand how these terms affect your practice's revenue, and flag issues that you can use to create leverage during negotiations.
Benchmarking
After you audit your current insurance contract terms, you must perform market rate analysis to benchmark your insurance reimbursement rates against Medicare and market standards.
Medicare is a universal benchmark. Reimbursement rates follow federal law. Therefore, the annually published Physician Fee Schedule serves as a valuable reference point for comparing payer reimbursement rates. Many commercial insurance companies express rates as a percentage of Medicare. For example, your contract may express a rate for a specific CPT code as 110 percent of Medicare, meaning the payer reimburses 110 percent of what Medicare would pay.
Compare your contract rates to current Medicare rates. Any rate below 100 percent of Medicare indicates that it's below industry norms.
Don't stop with Medicare benchmarking. It's also important to compare your practice's rates with local and national benchmarks. CMS now requires all payers to publish all negotiated rates each month into Machine Readable Files. Several firms, including Fuse, offer services to help analyze this data to benchmark your rates against competitors.
Proven Strategies for Higher Insurance Payments
Payer contract optimization can be daunting. However, if you take the time to prepare and collect data, you can easily develop a strategy that works in your practice's favor. There are many tactics you can employ. Let's explore some of the most effective.
Get Higher Insurance Payments By Leveraging Patient Volume
Volume-based rate increases are another strategy that practices can leverage to great success. Payers are more likely to increase reimbursement rates if a practice can demonstrate that it serves a significant number of in-network patients. Insurance companies don't want to lose patients if a practice decides to leave a network. Therefore, considerable volume is a powerful bargaining chip.
Here's where data collection and analysis make a difference. During your negotiations, prove that your practice can drive referrals and reduce out-of-network leakage. Demonstrate that your practice is a go-to for a payer's members in your area, and highlight how leaving the network could impact the payer's bottom line. Utilize billing reports and EMR data to demonstrate the value of your practice.
That data can be the tipping point for insurance companies. You may even have enough leverage to propose a tiered rate increase. Tie insurance reimbursement rate increases to patient volume benchmarks. This approach reframes negotiations, turning your request for increased rates into a mutually beneficial arrangement.
Propose Multi-Year Agreements with Incremental Increases
Rather than asking for immediate improvements to your medical provider contracts, you can propose multi-year agreements with smaller annual rate increases. This strategy is often more successful than sudden rate increases, as it allows payers to adjust terms over time while securing your in-network partnership for a longer period.
Consider proposing a multi-year agreement with a clause that covers predetermined rate escalators. For example, you can agree to a five-year contract with annual rate increases of 2 to 4 percent. This type of agreement will protect your practice from inflation and increasing operating costs. More importantly, it prevents rate stagnation while providing more predictable revenue.
When developing your proposal, use patient volume data to demonstrate that your practice will continue to be a valuable asset to the payer's network.
Highlighting the Value Your Practice Provides to Create a Win-Win Scenario for Payers
Does your practice offer something that others can't? If so, use it to negotiate insurance contract rates that increase your revenue potential. Think about what sets your practice apart from the competition.
One of the most common bargaining chips is scarcity. For example, your practice might offer family care in a Medically Underserved Area. If your practice serves a remote location without many providers for patients to turn to, you have more bargaining power than you might realize.
Another common scenario is that you offer a specialty that few others in the geographic region do. Patients often prefer not to drive hours to see a specialist. If you're the only neurosurgeon in town, payers are more likely to increase reimbursement rates to keep you in-network.
Approaching Insurance Companies: Preparation Phase
We've already covered the importance of collecting and analyzing data. However, you must strategically present that information to ensure that you have all the necessary bargaining power to achieve success.
Before approaching insurance companies, gather data on practice performance, patient volume and other relevant metrics. Payers want to see value. When you can show that your practice provides value to the insurance network, you're more likely to get better insurance reimbursement rates.
Volume is always important. However, our data should also reflect clinical outcomes and the overall patient experience. Participate in CMS programs, score high on CAHPS surveys and collect data that shows positive patient outcomes. Lower hospital readmission rates, reduced infection rates, a higher volume of screenings, more frequent preventative care and other critical metrics can showcase that your practice is making a difference. You can even showcase great patient reviews your practice receives online.
Your goal is to show that your practice provides value that aligns with a payer's priorities. A payer's priorities are to deliver value-based care while improving patient outcomes. If you can prove that your practice does that, you have a strong case for better insurance contract terms.
It's also vital that you perform competitor analysis. Show how your rates, performance and patient outcomes compare to competitor practices, especially those that are within a payer's network.
The Centers for Medicare & Medicaid Services (CMS) requires that all payers publish their negotiated rates. That data lives in massive datasets called Machine-Readable Files (MRFs). Companies like Fuse can extract, interpret and benchmark negotiated rates, providing actionable insights and information that practices can use during rate negotiations.
Study that data to build your case and include it in a clear and concise proposal packet. These packets should provide strong evidence of value that justifies your insurance reimbursement rate increase.
Maximizing Insurance Reimbursement Rates Through Strategic Timing
Proper timing can make or break your success when you negotiate insurance contract rates. When determining the optimal time to initiate negotiations, consider budget planning periods and renewal cycles.
Most insurance companies finalize annual budgets in late Q3 or early Q4. It's best to propose new insurance contract terms when payers finalize their budgets. If you do so afterward, there will be less flexibility from payers. Therefore, you have less leverage.
Contracts typically last one to three years. The best time to renegotiate terms is approximately three to six months before renewal. Any sooner, and you won't have much bargaining power. However, if you wait too long, you risk a tight negotiation schedule that may not reach its conclusion before your contract automatically renews at inferior rates.
The best approach is to develop and maintain a renewal schedule. Prepare early and create data-rich proposal packages you can submit at the right time.
Finally, consider how often you request negotiations. If you recently received an increase in insurance reimbursement rates in the last year, it's more challenging to get payers to engage in discussions. You don't want to request increases too often.
Remain Human
Our last tip is an easy one: Be kind and remain professional when negotiating with payer reps. It always pays to develop a rapport with the representatives you interact with. Build a strong professional relationship from the start, and representatives are more likely to engage with you when it's time to renegotiate insurance contract terms.
It's always good to remain firm. You want to do what's best for your practice. However, never approach negotiations from a place of hostility. That rarely works in a practice's favor, often backfiring. Instead, be cordial and present your case with data. Data-backed proposals pack a more potent punch than any form of aggression. Show payers precisely why your practice deserves better rates, backing everything you propose with concise data.
Transform Your Practice Revenue with Expert Contract Support
Negotiating an increase in reimbursement rates can be a challenging process that requires significant preparation and thorough data analysis. However, your practice doesn't have to approach negotiations alone. Expert analysis and support can give you a competitive edge, ensuring you have as much bargaining power as possible.
Fuse can provide expert guidance when navigating complex payer relationships. Fuse can automate patient intake and perform CPT code-level insurance verification. With Fuse, practices like yours can significantly reduce administrative friction while potentially achieving a return on your professional assistance investment. When it comes time for your practice to negotiate insurance contract rates, Fuse can analyze, interpret and benchmark data within MRFs, providing you with all the information you need to negotiate better contract terms with confidence. Not only can Fuse support negotiations with data, but it can also offer additional services, such as intake, verification, and more.
Schedule your demo with Fuse today to learn more about how it can transform your practice and empower you with the data needed to negotiate insurance contract rates that lead to more revenue.
Complete Guide to Negotiate Insurance Contract Rates for Medical Practices
The Problem
When a patient walks into a US healthcare clinic today, they typically have no idea what they're going to pay. Unlike buying groceries, booking a hotel, or purchasing anything else in the modern economy, healthcare remains a financial black box. You receive treatment first, then wait weeks for a bill that often comes as a complete surprise.
This isn't just inconvenient—it's a significant financial risk for patients, and a symptom of a broken system. Only one in six patients know what their care will cost before treatment, despite the fact that twenty cents of every dollar healthcare providers spend goes to financial administration—not patient care, not medical equipment, but paperwork, phone calls, and bureaucracy.
The situation is increasingly unsustainable. Patients are walking into medical appointments with no idea what they'll owe, while healthcare costs continue rising at unsustainable rates. Meanwhile, providers lose up to 10% of their revenue to billing errors and underpayments.
Our Solution
We started Fuse because AI and other technologies can now automate many of the manual tasks that previously made accurate patient cost estimates nearly impossible to create efficiently.
Before, provider admin teams had to manually read insurance card details, contact patients for missing information, upload this data to payer websites, note patient benefits, call payers for additional details, read their contracts, calculate bills, explain bills to patients, before finally billing a patient. This process was slow, error-prone, and expensive.
Fuse is now automating these steps:
- Patient intake and data capture - automatically extracting and organizing insurance information
- Real-time insurance verification - conducting CPT-code level benefits checks without manual payer portal navigation
- Contract analysis and payment benchmarking - determining accurate allowed amounts and patient responsibility
- Automated cost estimation - generating precise patient estimates before treatment
- Streamlined billing and collections - handling the entire billing workflow
The results: We've already reduced insurance verification administration by over 95% while eliminating eligibility-related denials for our partners.
Our Vision
Every patient should know the accurate cost of their care before treatment—just like shopping for products anywhere else. This should be the norm, not the exception.
Patients should expect price transparency from their healthcare providers. Healthcare providers shouldn't have to spend hours determining the cost of care for each patient. When you buy anything else, you see the price upfront. Healthcare should work the same way.
We're building the infrastructure to make this vision reality. A healthcare system where financial transparency is standard, where patients can make informed decisions about their care, and where providers can focus on healing instead of endless administrative tasks.
As repeat entrepreneurs focused on financial inclusion, we're excited to be backed by leading investors like Y Combinator to make this vision a reality.
Why We Started Fuse: Fixing US Healthcare's Opacity
How Do Mental Health Counseling Costs in Anchorage Compare
If you're seeking mental health counseling in Anchorage, you're probably wondering what it will actually cost you. Unfortunately, the answer isn't straightforward; it depends heavily on your insurance plan and where you go for treatment.
A typical mental health counseling journey may involve three main services: an initial psychiatric evaluation to assess your condition ($129–$216 with insurance), extended psychotherapy sessions for in-depth treatment ($90–$195 per session), and psychological testing when needed for diagnostic clarity ($136–$219 per session). Most patients attend counseling sessions weekly for several months, so understanding these costs up front can help you budget for treatment and choose the most affordable provider for your situation.
How much you pay with insurance depends on several details: It varies based on whether you've met your deductible, what your plan charges for copays and coinsurance, and if your plan uses a flat copay or a percentage (coinsurance) for each type of mental health service. For example, if your deductible isn't met, you'll pay the full negotiated rate—say, $195 for extended psychotherapy. If your deductible is paid, you might just owe a $30 copay or 20% coinsurance (so $39 for a $195 session), depending on your plan. These details mean your out-of-pocket cost can change even for the exact same service at the same clinic.
Without insurance, you'll pay significantly more—typically $250–$400 for evaluations and $200–$410 per treatment session. Below, we'll break down the specific costs for each type of service you're likely to encounter.
What should you expect to pay for mental health counseling with insurance?
In-network mental health counseling costs in Anchorage, Alaska, are based on negotiated rates between your insurance company and providers, which represent the maximum amount your insurer will pay for covered services. Based on our analysis of negotiated rate contracts from Alaska-based providers for three major insurers, Aetna offers the lowest rates across most services while Moda provides significantly lower pricing but with very limited network access.
Insurance Coverage Comparison for Mental Health Counseling in Anchorage, Alaska
CPT 90791 — Psychiatric Diagnostic Evaluation
- Aetna: $200.81
- Premera: $216.05
- Moda: $129.00
CPT 90837 — Psychotherapy, 60 minutes
- Aetna: $170.75
- Premera: $194.73
- Moda: $90.00
CPT 96130 — Psychological Testing Evaluation (1st hour)
- Aetna: $136.46
- Premera: $219.12
- Moda: N/A
Sample Size
- Aetna: 259 providers
- Premera: 529 providers
- Moda: 2 providers
Analysis limited to three major payers and does not reflect rates from all available insurance options in Anchorage, Alaska.
Aetna offers the most competitive rates for both psychiatric evaluation services (CPT 90791) at $200.81 and extended psychotherapy sessions (CPT 90837) at $170.75. However, Premera provides moderate pricing across services with the largest provider network. The substantial difference in Moda's pricing may reflect their smaller provider network in Anchorage, Alaska, with only 2 contracted providers compared to Premera's 529.
Why do rates vary so much?
Mental health counseling rates in Anchorage vary so much because:
- Each insurance company negotiates different rates with providers, leading to wide differences in costs.
- Smaller provider networks (like Moda) may pay clinics higher rates to attract participation, while larger networks (like Premera) negotiate lower rates.
- Different CPT codes pay different amounts based on the service's complexity and time requirements.
In short, rates reflect insurance negotiations, network size, Alaska's higher medical costs, and service complexity.
What should you expect to pay without insurance?
Alaska Statute 18.23.400 requires healthcare providers to publish their standard charges for common procedures. These rates typically represent the full cost of services when insurance is not used.
Select Mental Health Providers in Anchorage, Alaska
Fireweed Counseling & Wellness (4.3/5, 6 reviews)
- CPT 90791: $395.00
- CPT 90837: $295.00
- CPT 96130: Not listed
Lantern Counseling (No rating data)
- CPT 90791: $275.00
- CPT 90837: $200.00
- CPT 96130: Not listed
Alaska Telepsychology (No rating data)
- CPT 90791: $409.72
- CPT 90837: $363.94
- CPT 96130: $350.75
White Wave Counseling (5.0/5, 1 review)
- CPT 90791: Not listed
- CPT 90837: $230–$275
- CPT 96130: Not listed
Bridges Counseling (2.7/5, 39 reviews)
- CPT 90791: Not listed
- CPT 90837: Not listed
- CPT 96130: Not listed
North Star Behavioral Health (1.7/5, 135 reviews)
- CPT 90791: Not listed
- CPT 90837: Not listed
- CPT 96130: Not listed
Alaska Behavioral Health (2.4/5, 37 reviews)
- CPT 90791: Not listed
- CPT 90837: Not listed
- CPT 96130: Not listed
Lantern Counseling publishes transparent pricing for evaluations at $275.00 for CPT 90791, while Alaska Telepsychology charges $409.72 for evaluations but offers comprehensive rates for psychotherapy at $363.94 and psychological testing at $350.75. Fireweed Counseling & Wellness offers standardized evaluation rates of $395.00 and psychotherapy sessions at $295.00 for their counseling services in Anchorage, Alaska.
Based on our research, several Anchorage mental health providers have implemented online rate transparency in compliance with Alaska law AS 18.23.400. Patients should contact providers directly to request Good Faith Estimates, which are legally required to be provided within specific timeframes.
How can you get accurate cost estimates for mental health counseling in Anchorage?
The most reliable way to determine your mental health counseling costs is to request a Good Faith Estimate from your chosen provider before treatment begins. Under Alaska Statute 18.23.400, providers must provide these estimates within ten days after receiving a request for non-emergency healthcare services.
This Alaska requirement differs from the federal Good Faith Estimate requirements under the No Surprises Act, which apply to uninsured and self-pay patients with different timelines: within one business day if scheduled 3–9 days in advance, or within three business days if scheduled 10 or more days in advance. Alaska's law provides a longer response timeframe but applies more broadly to all patients requesting estimates.
Disclaimer
The rate information presented in this article is derived from publicly available Machine Readable Files (MRFs) provided by insurance payers. This analysis focuses on select insurers and will not reflect rates from all available insurance options. While Fuse makes every effort to provide accurate and current information, healthcare pricing can change frequently, and individual circumstances may affect actual costs. This information should not be considered a guarantee of specific pricing. Patients should always contact their healthcare providers directly to request Good Faith Estimates and verify current rates before receiving treatment.
Anchorage Behavioral Therapy Costs by Insurance
Fuse recently had the opportunity to attend and present at the Alaska chapter of the Medical Group Management Association (MGMA) conference—a key gathering for forward-thinking healthcare leaders seeking solutions in cost management and technology. Our co-founders, Sho Sugihara and Oscar Wilsby, spoke on the transformative impact of Machine Readable Files (MRFs) mandated by CMS’s Transparency in Coverage Rule, emphasizing their pivotal role in making healthcare pricing both fair and transparent for patients and providers.
Why Machine Readable Files Matter
MRFs, first required in July 2022, offer unprecedented insight into both in-network and out-of-network rates, publicly surfacing negotiated prices for medical procedures nationwide. Fuse’s talk highlighted how this data, when processed properly, allows for apples-to-apples comparisons, empowering providers to benchmark contract rates and patients to better predict out-of-pocket costs. This advance brings us closer to a healthcare system where pricing is no longer a black box.
Doing the Heavy Lifting
At Fuse, we’re committed to making these enormous, complex datasets actionable. Our solutions take on the heavy lifting: downloading hundreds of gigabytes, untangling payer quirks, and filtering out “zombie rates” and data noise. While MRF data is an incredible opportunity, it has limitations—ambiguities, contract exclusions, and technical hurdles do exist, and careful clean-up is essential. Our goal is to give consumers, providers, and payers usable, trustworthy pricing information without glossing over what’s challenging about the data.
Making Healthcare Fair for All
As we shared at MGMA Alaska, the future of healthcare pricing is bright if MRF data can be vetted and presented cleanly. This transformation will allow providers to negotiate fairly and patients to choose care with confidence. We’re excited to be driving this progress and are always eager to collaborate with organizations and experts making healthcare more transparent and equitable.
If you’d like a copy of our presentation or wish to discuss Fuse’s approach to MRF data and price transparency, please get in touch!
Fuse Presents at 2025 MGMA Alaska Conference
Press Release
San Francisco, CA — Fuse, the healthcare technology startup, is proud to announce that co-founders Sho Sugihara (CEO) and Oscar Wilsby (CTO) have joined the Summer 2024 batch at Y Combinator, beginning July 2024.
Widely regarded as the world’s most selective and influential startup accelerator, Y Combinator has a strong track record of backing transformative companies across industries—including healthcare firmslike DrChrono and Athelas. The selective nature of Y Combinator’s application process means only a small fraction of startups earn the opportunity to join, placing Fuse among a distinguished group of global innovators.
“We’re honoured to be part of a program that has propelled so many market-leading companies, including pioneers in healthtech,” said Sho Sugihara, CEO and Co-Founder of Fuse. “With Y Combinator’s support, we’re excited to accelerate our mission to address healthcare’s greatest challenges.”
Fuse’s acceptance into Y Combinator brings access to a world-class network of investors, mentors, and industry leaders. As alumni of the accelerator, Sugihara and Wilsby will gain new platforms to advance Fuse’s vision for healthcare workforce innovation—joining the ranks of influential startups that have shaped industries worldwide.
For more information about Fuse and its solutions, visit the company website.
Fuse Joins Y Combinator’s Summer 2024 Cohort
Press Release:
Las Vegas, NV — Fuse, a healthcare technology innovator, has been recognized as a Winner’s Circle startup in the Hospital Systems – Workforce/Staffing Shortages category at the HIMSS Emerge Innovation Experience Contest 2025. This annual event, one of the largest conferences in healthcare and hosted at the HIMSS Global Health Conference, spotlights forward-thinking solutions that address critical challenges facing the healthcare sector.
As part of the Winner’s Circle, Fuse earned selection for its impact in supporting healthcare providers to solve staffing and workforce shortages—one of the most urgent issues in care delivery. Winner’s Circle honorees are celebrated with special event recognition, curated meetings with healthcare C-suite leaders, and inclusion in HIMSS’s post-conference global marketing, providing platforms for further collaboration and visibility in the healthcare ecosystem.
“We’re honoured to be included alongside so many outstanding innovators,” said Sho Sugihara, CEO and Co-Founder of Fuse. “At a time when provider workforce challenges are at the forefront, this recognition affirms the value of our work and drives us to keep advancing real-world solutions.”
A full list of winners is available in the official announcement from HIMSS at: https://www.himssconference.com/wp-content/uploads/2025/02/EmergeWinners2025.pdf. Learn more about the Emerge Innovation Experience: https://www.himssconference.com/emerge-innovation-experience/.
For more information about Fuse and its solutions, visit the website.
Fuse Joins Winner’s Circle at HIMSS 2025 for Addressing Workforce Shortages
Press Release:
Nashville, TN — Fuse, a healthcare technology company, was named the winner of the ViVE 2025 Startup Pitch Competition, an event that spotlights promising new solutions in digital health. The competition, held during the ViVE Event in Nashville, brought together startups from across the industry to share advancements aimed at improving healthcare delivery.
Fuse’s solution was selected by a panel of industry experts for its potential to support better price transparency for patients and contribute meaningfully to the healthcare ecosystem. As part of this recognition, Fuse will receive a $25,000 cash prize from HLTH and a $25,000 credit toward ViVE 2026.
“We’re grateful to the ViVE organizers and judges for this opportunity,” said Sho Sugihara, CEO and Co-Founder of Fuse. “It’s an honor to be included alongside so many innovative companies, and we’re excited to continue our work in collaboration with the broader healthcare community.”
The ViVE Startup Pitch Competition, along with the AgeTech Pitch presented by AARP’s AgeTech Collaborative™, highlights emerging talent and creative approaches to challenges in health and aging.
For more information about Fuse and its initiatives, visit the website.
Fuse Wins ViVE 2025 Pitch Competition for Price Transparency Innovation
How Do Physical Therapy Costs in Anchorage Compare
If you're seeking physical therapy in Anchorage, you're probably wondering what it will actually cost you. Unfortunately, the answer isn't straightforward; it depends heavily on your insurance plan and where you go for treatment.
A typical physical therapy journey may involve three services: an initial evaluation to assess your condition ($99–$301 with insurance), therapeutic exercises to build strength and mobility ($45–$88 per session), and hands-on manual therapy for pain relief ($45–$81 per session). Most patients attend PT 2-3 times per week for 4-8 weeks, so understanding these costs up front can help you budget for treatment and choose the most affordable provider for your situation.
How much you pay with insurance depends on several details: It varies based on whether you've met your deductible, what your plan charges for copays and coinsurance, and if your plan uses a flat copay or a percentage (coinsurance) for each type of physical therapy service. For example, if your deductible isn’t met, you’ll pay the full negotiated rate—say, $58 for therapeutic exercise. If your deductible is paid, you might just owe a $30 copay or 20% coinsurance (so $12 for a $58 session), depending on your plan. These details mean your out-of-pocket cost can change even for the exact same service at the same clinic.
Without insurance, you'll pay significantly more—typically $200–$350 for evaluations and $95–$120 per treatment session. Below, we'll break down the specific costs for each type of service you're likely to encounter.
What should you expect to pay for physical therapy with insurance?
In-network physical therapy costs in Anchorage, Alaska, are based on negotiated rates between your insurance company and providers, which represent the maximum amount your insurer will pay for covered services. Based on our analysis of negotiated rate contracts from Alaska-based providers for three major insurers, Aetna offers the lowest evaluation rates while Premera provides more competitive pricing for treatment services.
Insurance Coverage Comparison for Physical Therapy in Anchorage, Alaska
- CPT 97161 — PT Evaluation
- Aetna: $99.02
- Premera: $133.65
- Moda: $301.00
- CPT 97110 — Therapeutic Exercise (15 min)
- Aetna: $58.10
- Premera: $47.85
- Moda: $87.40
- CPT 97140 — Manual Therapy (15 min)
- Aetna: $53.78
- Premera: $44.00
- Moda: $80.38
- Sample Size
- Aetna: 391 providers
- Premera: 1,008 providers
- Moda: 22 providers
Analysis limited to three major payers and does not reflect rates from all available insurance options in Anchorage, Alaska.
Aetna offers the most competitive rates for physical therapy evaluation services (CPT 97161) at $99.02, making them significantly more affordable than Moda's rate of $301.00. However, Premera offers the lowest rates for both therapeutic exercise (CPT 97110) at $47.85 and manual therapy (CPT 97140) at $44.00. The substantial difference in Moda's pricing may reflect their smaller provider network in Anchorage, Alaska, with only 22 contracted providers compared to Premera's 1,008.
Why do rates vary so much?
Physical therapy rates in Anchorage vary so much because:
- Each insurance company negotiates different rates with providers, leading to wide differences in costs.
- Smaller provider networks (like Moda) may pay clinics higher rates to attract participation, while larger networks (like Premera) negotiate lower rates.
- Different CPT codes pay different amounts based on the service's complexity.
In short, rates reflect insurance negotiations, network size, Alaska’s higher medical costs, and service complexity.
What should you expect to pay without insurance?
Alaska Statute 18.23.400 requires healthcare providers to publish their standard charges for common procedures. These rates typically represent the full cost of services when insurance is not used.
Select Physical Therapy Providers in Anchorage, Alaska
- Empower Physical Therapy (5/5, 310 reviews)
- CPT 97161: $225.00
- CPT 97110: $110.00
- CPT 97140: $95.00
- Runners' Edge Alaska (5/5, 65 reviews)
- CPT 97161: $350.00
- CPT 97110: $105.00
- CPT 97140: $95.00
- Integrative Physical Therapy (4.9/5, 85 reviews)
- CPT 97161: $216.00
- CPT 97110: $108.00
- CPT 97140: $83.00
- United Physical Therapy (5/5, 163 reviews)
- CPT 97161: $295.00
- CPT 97110: $121.00
- CPT 97140: $120.00
- Advanced Physical Therapy (4.9/5, 185 reviews)
- CPT 97161: $260.00
- CPT 97110: $98.00
- CPT 97140: $93.00
Empower Physical Therapy publishes transparent pricing for evaluations at $225.00 for CPT 97161, while Runners' Edge Alaska charges $350.00 for evaluations but offers competitive rates for therapeutic exercise at $105.00 and manual therapy at $95.00. All For Kids Pediatric Therapy offers standardized evaluation rates of $260.00 and therapeutic exercises at $90.00 for their specialized pediatric services in Anchorage, Alaska.
Based on our research, several Anchorage physical therapy providers have implemented online rate transparency in compliance with Alaska law AS 18.23.400. Patients should contact providers directly to request Good Faith Estimates, which are legally required to be provided within specific timeframes.
How can you get accurate cost estimates for physical therapy in Anchorage?
The most reliable way to determine your physical therapy costs is to request a Good Faith Estimate from your chosen provider before treatment begins. Under Alaska Statute 18.23.400, providers must provide these estimates within ten days after receiving a request for non-emergency healthcare services.
This Alaska requirement differs from the federal Good Faith Estimate requirements under the No Surprises Act, which apply to uninsured and self-pay patients with different timelines: within one business day if scheduled 3–9 days in advance, or within three business days if scheduled 10 or more days in advance. Alaska's law provides a longer response timeframe but applies more broadly to all patients requesting estimates.
Disclaimer
The rate information presented in this article is derived from publicly available Machine Readable Files (MRFs) provided by insurance payers. This analysis focuses on select insurers and will not reflect rates from all available insurance options. While Fuse makes every effort to provide accurate and current information, healthcare pricing can change frequently, and individual circumstances may affect actual costs. This information should not be considered a guarantee of specific pricing. Patients should always contact their healthcare providers directly to request Good Faith Estimates and verify current rates before receiving treatment.


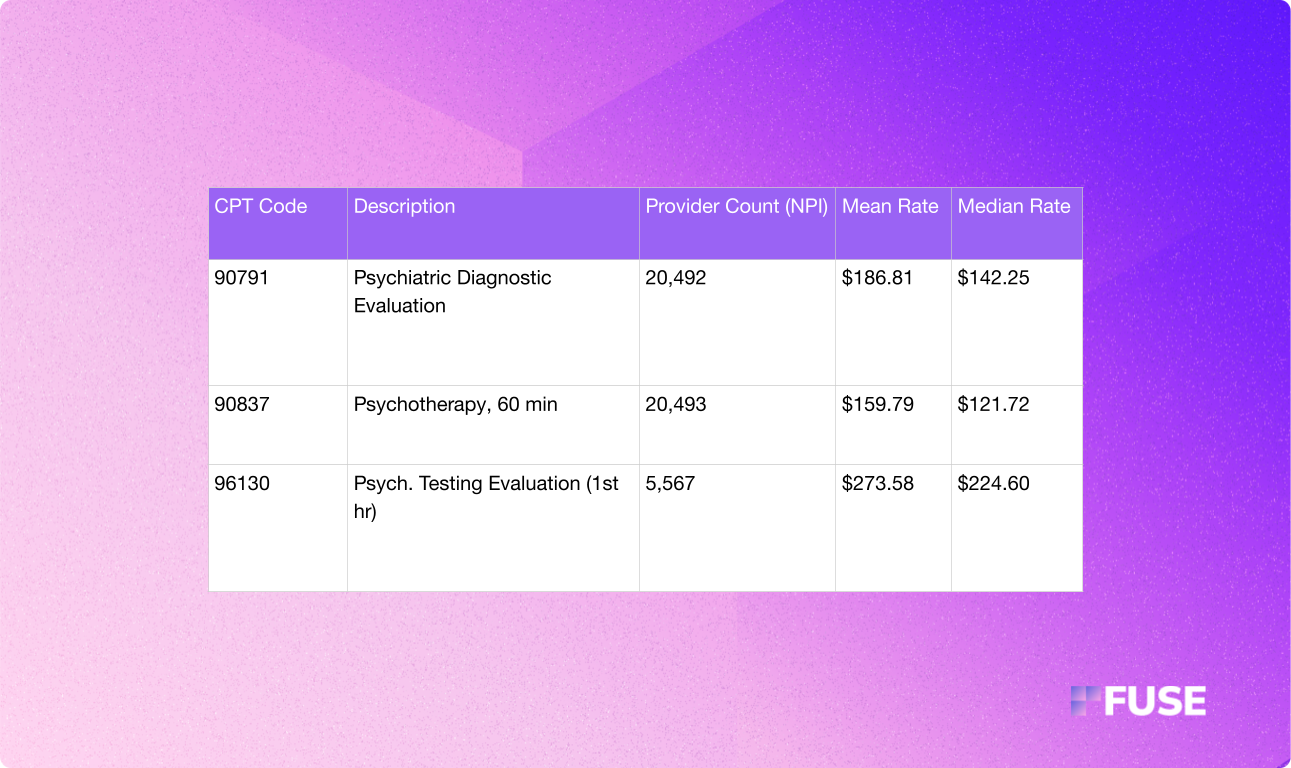
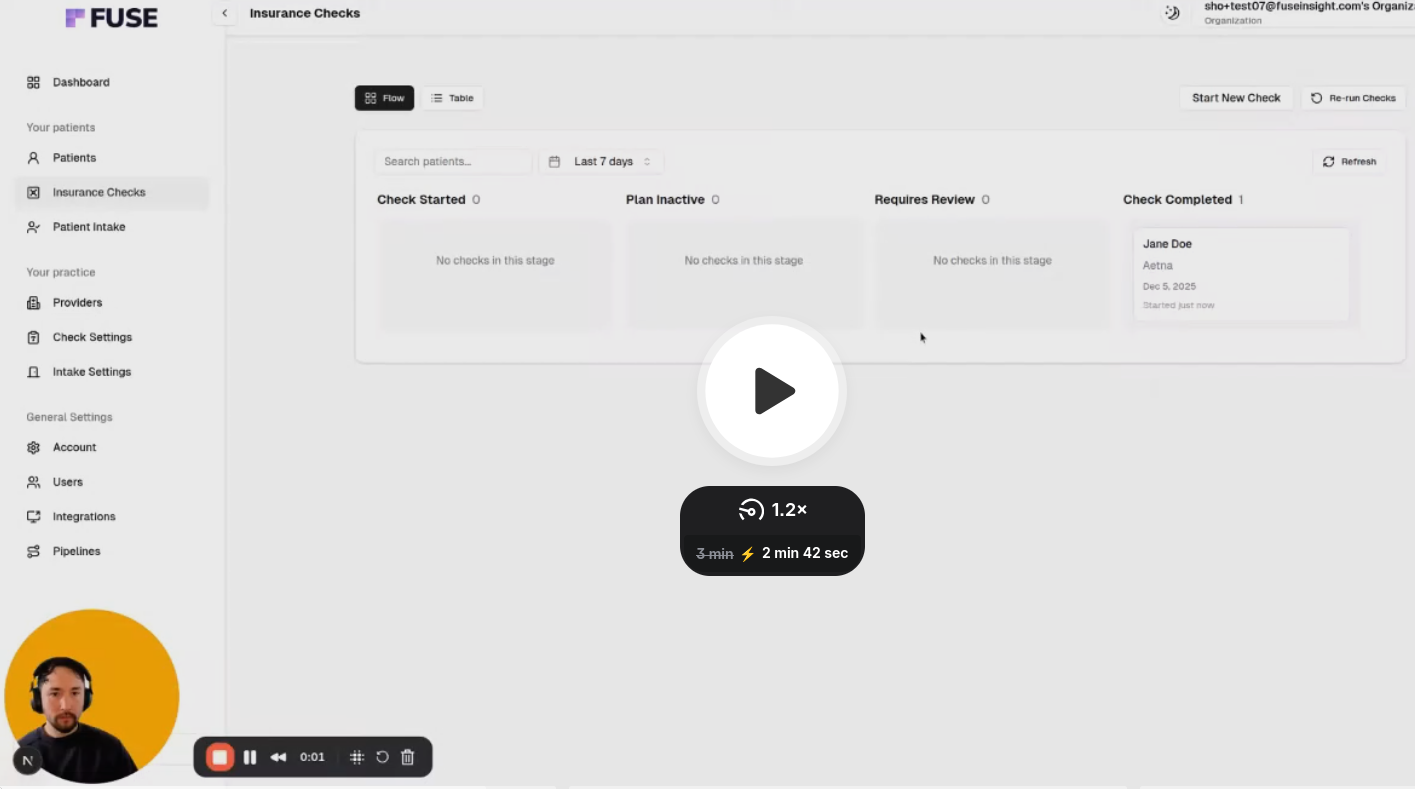

.avif)
.avif)
.avif)

.avif)
.avif)


