Real-Time Eligibility Checks with Automated Insurance Verification
Manual insurance verification is painful, prone to errors and causes delays to patient intake, while causing costly claim denials when done wrong. Fuse automates the entire insurance eligibility verification process at the CPT code level, eliminating errors and freeing your team to focus on patient care.
SCHEDULE A DEMO
Hours Saved
Auto-generate billing summaries and insurance verification results at the CPT code level, confirming coverage details and network status before visits while reducing administrative work and errors.
Insurance Eligibility Verification at CPT Level
Basic eligibility checks miss critical coverage details that cause claim denials. Fuse verifies benefits at the CPT code level, ensuring you know exactly what's covered for each procedure before appointments, such exact copays, coinsurance, visit limits and prior auth requirements.
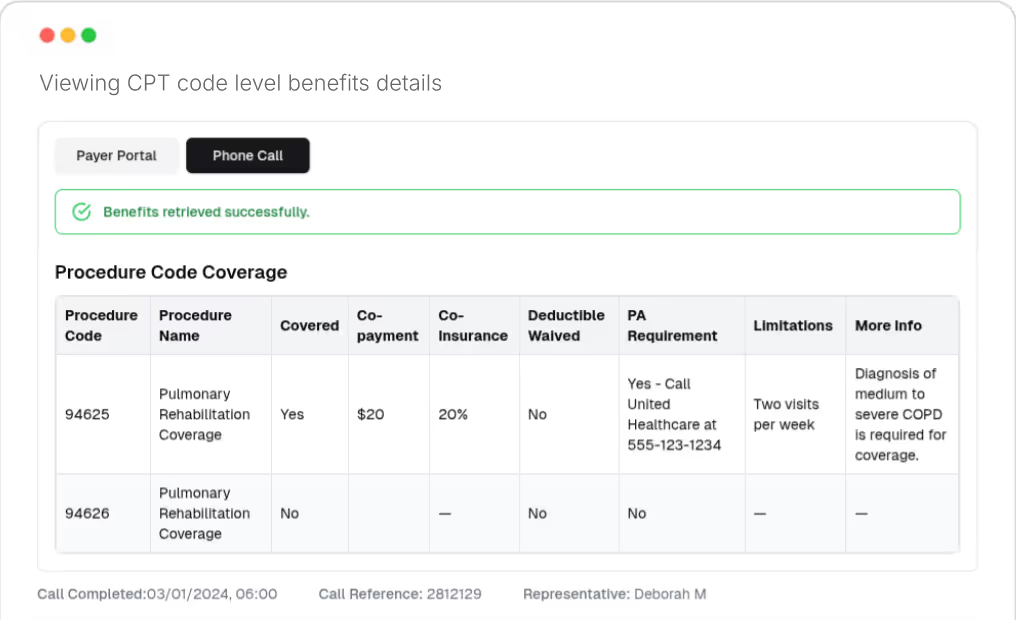
Portal Checks Plus Payer Calls for Maximum Accuracy
Payer portals provide basic information, but direct calls reveal specifics like prior authorization requirements and visit limits at the CPT code level. Fuse takes a dual approach by combining both methods to deliver complete, accurate benefits verification every time.
.avif)
Network Status Confirmation
Get confirmation of network status and coverage details before appointments through automated payer phone calls. Prevent out-of-network surprises and provide patients with upfront cost clarity they can trust.
.avif)
Reduce Administrative Burden and Errors
Eliminate manual lookups and hours spent on hold with payers. Fuse handles eligibility checks automatically, reducing verification errors by up to 95% while freeing staff to focus on patients instead of paperwork.
.avif)
After a short onboarding call, we start learning your existing workflows and customize our solution to minimize disruption to your team.
Insurance Eligibility Verification at CPT Level
Basic eligibility checks miss critical coverage details that cause claim denials. Fuse verifies benefits at the CPT code level, ensuring you know exactly what's covered for each procedure before appointments, such exact copays, coinsurance, visit limits and prior auth requirements.
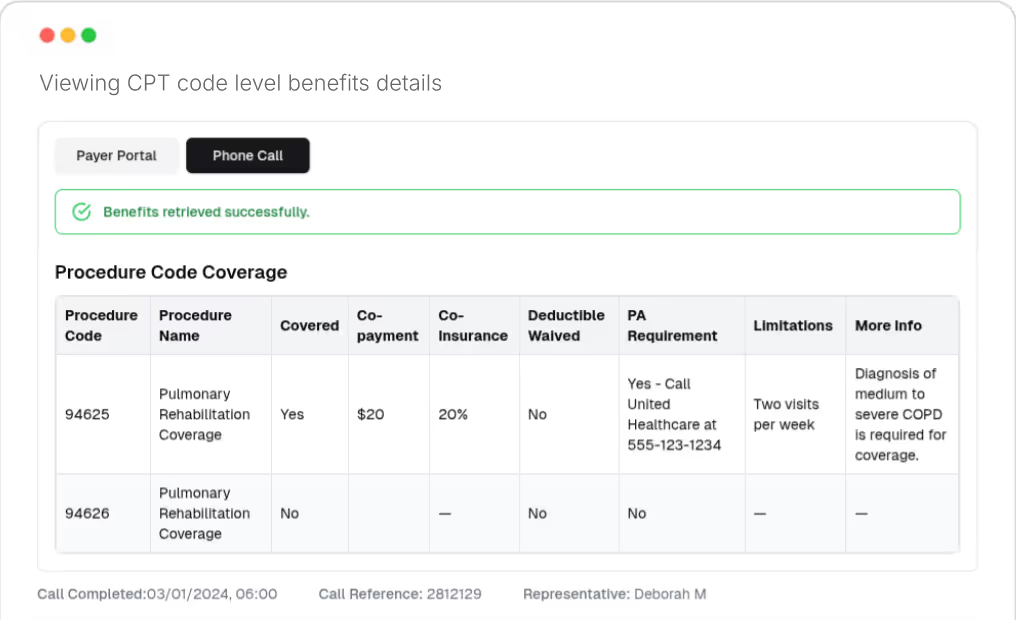
Portal Checks Plus Payer Calls for Maximum Accuracy
Payer portals provide basic information, but direct calls reveal specifics like prior authorization requirements and visit limits at the CPT code level. Fuse takes a dual approach by combining both methods to deliver complete, accurate benefits verification every time.
.avif)
Network Status Confirmation
Get confirmation of network status and coverage details before appointments through automated payer phone calls. Prevent out-of-network surprises and provide patients with upfront cost clarity they can trust.
.avif)
Reduce Administrative Burden and Errors
Eliminate manual lookups and hours spent on hold with payers. Fuse handles eligibility checks automatically, reducing verification errors by up to 95% while freeing staff to focus on patients instead of paperwork.
.avif)
HIPAA-Compliant Healthcare Automation Platform


GET INSURANCE
VERIFICATION RIGHT
THE FIRST TIME

FAQs
How does CPT code level verification improve accuracy?
CPT code level verification checks benefits for each specific procedure, not just general eligibility and coverage by STC (Service Type Code). This prevents claim denials caused by missing coverage details or authorization requirements for the specific procedure. It also helps identify the exact copays and coinsurance that a patient must pay for each procedure, which often cannot be determined on portals like Availity, pVerify or Office Ally. For example, these platforms may only state what a specialist visit copay is, and fall short of specifying the exact copay for an initial visit with a psychiatrist, or show multiple copay options.
Why combine portal checks with payer calls?
Portals provide basic coverage information, but calls reveal specifics like prior authorization requirements, visit limits, and the copays and coinsurances that apply to that specific CPT code. Payer calls can also help determine whether the billing provider is seen as a specialist by the specific payer, and how their specific qualification impacts patient benefits. Using both portals and calls ensures complete, accurate benefits verification.
How are payer discrepancies identified and resolved?
Fuse compares portal and call results to identify inconsistencies. Discrepancies are flagged for review in our dashboard and in the summary that we produce for each check that can be inputted into your EHR. Typically, we find that discrepancies occur when a payer rep gives incorrect information on benefits information. In this instance follow-up calls can be scheduled to clarify the correct benefit details.
Can this system identify coverage limitations?
Yes, Fuse identifies coverage limitations, prior authorization requirements, and visit limits at the CPT code level, reducing costly eligibility-related claims denials by pulling detailed benefit information from both payer portals and direct calls.
How can network status be confirmed?
Network status cannot be confirmed for most payers through automated portal checks. Most practices may have a sense of which plans they are in-network with, but for niche plans like self-insured plans run by a TPA, confirming network status can be trickier. Fuse uses direct verification calls to confirm network status and make sure there are no surprises when claims are adjudicated and patients need to be billed for rendered services.
How much time can I save by automating benefits checks?
Manual eligibility and benefits checks can take billing teams anywhere from 15 minutes to 2 hours depending on data complexity and payer hold times, with the checks we've done averaging about 30 minutes. That includes extracting data from the EHR, checking portals, calling payers, and adding a benefits note back to the patient account. Fuse automates this entire process, reducing administrative time by up to 95%, so the time and workload savings for teams can be significant.
What is the financial benefit of automating benefits checks?
The exact $ benefit will depend on each practice and patient volume. This said, we see three benefits: First, the admin overhead saved by your team no longer having to do benefits checks, which can amount to 30 min per patient. Second, we typically see up to 20% of denials being caused by incorrect eligibility checks. For example, missing a prior auth requirement, or billing outdated insurance for a patient who recently switched employers. Our checks can prevent these. Finally, faster checks can increase the speed and volume of patient intake and help grow revenue.

