These days, patients no longer leave their healthcare to chance or rely on basic referrals to find the care they need. Today's patients set the agenda, conducting more research about practices and providers than ever before in history. Their tool of choice? The Internet!
In 2023, approximately 5 percent of Google's daily search volume was health-related, a figure that's likely higher today. Recent surveys suggest that a vast majority of patients (roughly 77 percent) research online before booking appointments. One study found that over 90 percent of patients read provider bios and gather information about a practice before reaching out through official channels. That data highlights a significant shift in patient behaviors. People take an active role in finding the best care possible. To boost patient acquisition, your medical practice marketing needs to keep up.
Search engine optimization (SEO) is a digital marketing strategy that can lead to long-term growth and success for practices like yours. Strong SEO for medical practices can establish your website as a trusted authority, attracting potential patients and growing organic search traffic. Shifting focus toward SEO can make a difference. Estimates say that more than half of all visits to healthcare websites come from organic searches. While results can vary, numerous case studies demonstrate that effective SEO practices pack a punch. One case study showed that for every $1 spent on SEO, practices can net between $4 and $10 in revenue. In another case study, a practice increased organic search traffic by over 46 percent, resulting in a 16 percent increase in year-over-year appointment requests.
There's more than enough evidence to demonstrate that SEO is effective across various industries, including healthcare. However, medical practices have many unique challenges that other types of businesses don't. Numerous regulations impact how practices can advertise their services. There's a delicate balance between maintaining HIPAA compliance and meeting E-E-A-T requirements needed to maximize online visibility. In this guide, we'll explore the importance of SEO for medical practices and provide game-changing strategies that can help you attract more patients while setting your practice up for long-term growth.
Why Healthcare SEO Optimization Drives More Patient Conversions
Search engine optimization is all about building a strong, authoritative online presence. This strategy involves optimizing your website for search engines, making it appear as high as possible on search engine result pages (SERPs). It aligns with modern patient behaviors, presenting your practice as the best choice for their needs, while also providing relevant information that goes into their decision-making.
There are many reasons why healthcare SEO optimization is so effective. However, it all revolves around trust. When patients are looking for providers and practices, several key factors influence their decision-making process, and medical practice SEO can have a bigger impact than you may realize.
• Higher Rankings: Did you know that over 75 percent of people never go beyond Google's first page of results? Most people trust search engine algorithms to deliver high-quality results. Therefore, having your practice's page appear high up on the first page automatically signals reliability.
• Reviews Positive reviews matter. Not only do most patients read them before booking an appointment, but reviews can also influence rankings. Practices with high online visibility and positive ratings are more likely to convert searchers into patients.
• Website Professionalism: SEO ranking factors like mobile optimization, website speed and UX design help put the best websites at the top of a results page. Part of medical practice SEO is having a modern, easily accessible website that patients will enjoy visiting. In addition to helping you rank higher, a well-built and optimized website will reflect positively on your practice. It signals professionalism, another major trust factor that can influence patient choices.
• Authoritative Content: SEO for medical practices involves more than just using keywords throughout your content. Your strategy should emphasize high-quality content that establishes experience, expertise, authoritativeness and trustworthiness (E-E-A-T). Publishing content that meets E-E-A-T guidelines will lead to improved rankings. More importantly, it helps build trust among potential patients.
• Local SEO: Because most patients are looking for local healthcare providers, prioritizing local SEO for doctors and practices can lead to measurable improvements. Searches containing "near me" have reportedly increased by over 500 percent in the last few years, primarily driven by the widespread use of mobile devices. One study found that 42 percent of people making local searches click on one of the results that appear on a Google Map Pack, highlighting the importance of local SEO and complete business profiles.
The ROI Benefits of Healthcare SEO Optimization
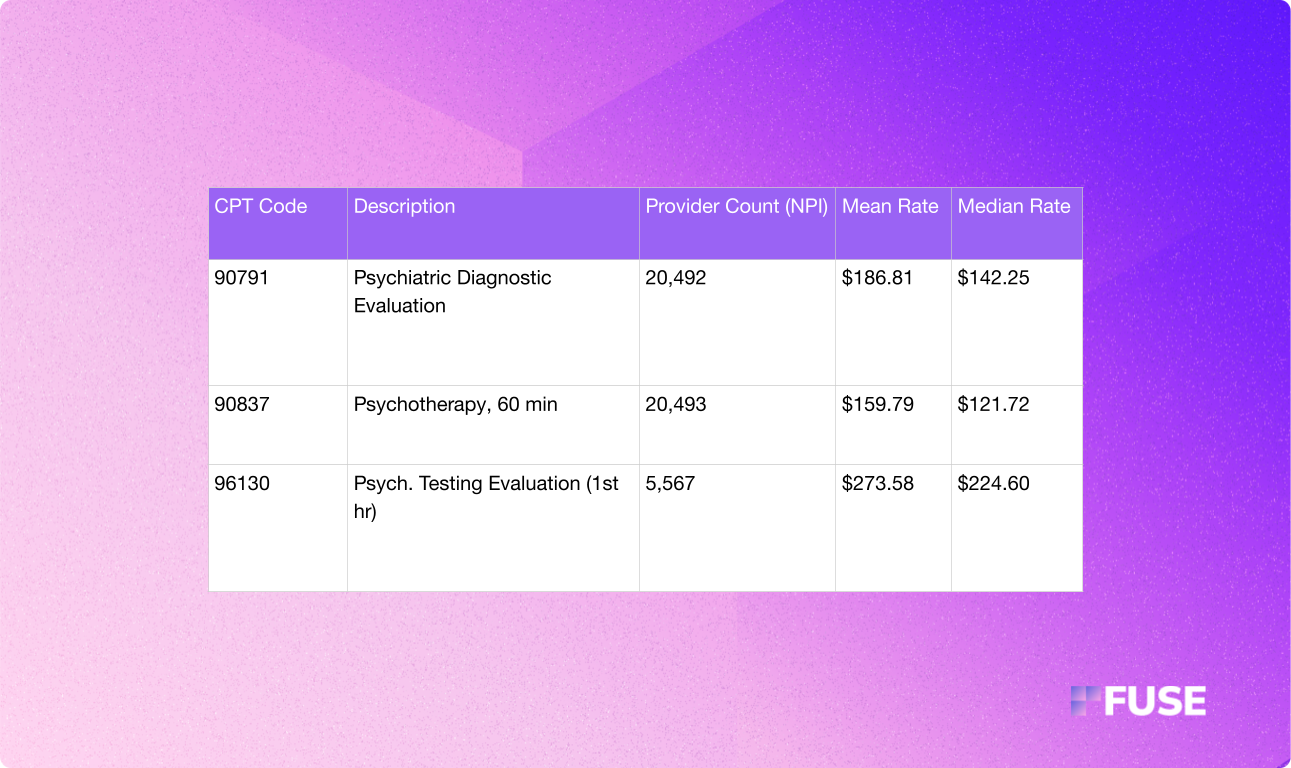
When you compare the costs of a robust SEO strategy to more traditional medical practice marketing techniques, SEO can provide a much better return on your investment. The average cost per patient acquisition can vary significantly depending on your market and level of competition. However, the average medical practice spends about $300 on SEO to acquire a new patient.
That's significantly less than what practices spend on other marketing channels. Specialty practices can expect to pay around $800 to acquire a single new patient through PPC ads on Google. Meanwhile, practices offering elective or cosmetic procedures can spend up to $1,500. Providers that incorporate television or radio ads can find themselves paying thousands to convert a single patient.
SEO is more cost-effective every way you look at it. But that's not all. The ROI for healthcare SEO optimization compounds, continually improving over time. Unlike paid ads, traffic doesn't disappear when spending stops. Your SEO efforts continue to pay off over time, making it easier to experience gradual growth while competing with larger systems that have bigger marketing budgets than your own.
Essential SEO for Medical Practices: Foundation Elements
Successful medical website optimization starts with a strong foundation. It can feel overwhelming, especially when up against larger healthcare systems with seemingly bottomless marketing budgets. However, the beauty of SEO is that it's accessible to practices of all sizes. What's important is that you take the time to get things right and set your site up for success.
SEO takes time. While paid ads and more conventional strategies can provide a temporary boost, strong medical SEO strategies are about the long game, building organic traffic that leads to continued success and visibility. We'll get into the importance of local SEO and high-quality content soon. However, for now, let's cover the basics.
• Speed Improvements: Ever try to use a website that was sluggish and slow to load? No one enjoys that, and search engines don't view poor performance favorably when developing rankings. Aim for a load time of less than three seconds by utilizing browser caching or a CDN. You can also prioritize over-the-fold content loading, compress images and more.
•Mobile Optimization: The latest estimates show that roughly 68 percent of all health searches occur on a mobile device. Mobile medical website optimization is a must. Search engines like Google use mobile-first indexing. Therefore, sites not optimized for mobile devices rank lower than those that are. You want to ensure your website is accessible on the go.
• Security: Search engines like Google prioritize secure websites using HTTPS. Successful healthcare SEO optimization requires that all pages utilize SSL to build trust and ensure patient information remains safe.
• UX Enhancements: A positive user experience can make a website stand out. Search engines rank websites based on their usefulness and relevance. When developing a medical practice SEO strategy, consider revamping your website to ensure easy, enjoyable navigation. Utilize menus for navigation, provide easy access to appointment booking forms and make all pages easy to find.
• Descriptive Tags and Descriptions: On-page SEO elements like title tags and meta descriptions matter. They help search engines understand your site and can influence a user's decision to click your link. Incorporate relevant keywords and location data to improve your healthcare digital marketing content.
• Schema Markup Implementation: Like tags and descriptions, schema markups help search engines understand what your website is all about. The right structured data on each page can lead to improved search result visibility.
• Internal Linking: Don't forget to link to other pages on your website. Internal linking can significantly improve site navigation and strengthen topical authority. It can also increase the amount of time visitors spend on your site, increasing the chances of conversion.
• AI-Ready Content Structure: Format content with clear headings, FAQ sections, and structured data markup. As AI-powered search grows, well-organized content that answers specific questions will be more likely to appear in AI responses and voice search results.
E-E-A-T Requirements for Medical Content
E-E-A-T is an acronym that reflects what Google's human quality raters consider when evaluating the credibility of online content. As mentioned earlier, E-E-A-T stands for experience, expertise, authoritativeness and trustworthiness. The specifics of the algorithm that Google uses to find and rank relevant websites are a mystery, and they frequently change to align with user needs. However, following E-E-A-T requirements is an excellent way to ensure you're creating content that search engines find favorable.
Embracing E-E-A-T is vital for all forms of digital marketing. However, things are different when implementing medical SEO strategies. Medical content falls under the "Your Money or Your Life" (YMYL) umbrella. YMYL is a collection of topics that Google applies higher standards to, as they could significantly impact a person's health, safety, happiness or financial stability.
When developing content, it is essential to keep E-E-A-T in mind. However, to ensure Google elevates your content instead of suppressing it to protect users from harm, you need to provide proof of E-E-A-T. To meet all E-E-A-T requirements for medical content, it needs to meet the following criteria:
• Content must be written or reviewed by qualified healthcare professionals to prove expertise.
• Content must be factually correct and backed by medical sources to build authority.
Websites and content must have transparent information about credentials, contact information and compliance to earn trust.
Medical Practice Marketing Through Local SEO Dominance
In medical practice marketing, local SEO is often more important than broader global SEO. Medical practices like yours serve people within your geographical area. While becoming an authority in your specialty on a worldwide scale is always beneficial, you want to focus your digital marketing resources toward local SEO dominance.
The first step is to complete your Google Business Profile (GBP). This free profile is often the first thing potential patients see about your practice. Optimizing it can significantly boost local search visibility.
Create a profile or claim an existing one for your business. Then, fill out every available section. Create an engaging description, provide information about your services, add photos and more, all while complying with those E-E-A-T requirements for medical content.
Once you complete your profile, you can work to earn citations and reviews to build your authority. It's also important to respond to any reviews you receive on Google. Remember: Most patients read reviews about healthcare providers and practices before booking an appointment. Negative reviews happen to every practice. What's critical is that you respond to them in a professional manner.
Respond to any reviews within 48 hours to show attentiveness. If the review is negative, acknowledge the reviewer's pain points, apologize for their experience and invite them to reach out to your practice to resolve the situation. When responding to negative or positive reviews, ensure your responses are HIPAA-compliant. For example, you should avoid confirming that the reviewer is a patient or responding with any potentially sensitive information.
Keep responses general and professional. Never respond with negativity, excuses or accusations! Always remember that people reading those reviews may become future patients. Keep your cool and remain cordial. After interacting with patients in your office, invite them to leave a Google review. Doing so can help you build up a positive reputation, ultimately benefiting your SEO efforts, while offsetting those occasional negative reviews you might receive.
Medical SEO Strategies for Google Business Profile
There are numerous ways that practices can optimize their Google profiles. Here are a few tips that can make all the difference in local search visibility.
• Complete Every Available Section: Don't leave any section blank. A complete profile is better for rankings. Include office hours, phone numbers, physical addresses, etc. You also want to provide a practice description that contains high-value keywords.
• Ensure Consistency: Triple-check that all names, addresses and phone numbers are consistent between your website, business profile and social media. Pay close attention to spelling and capitalization.
•List Available Services: List as many services as you can to cover all potential keywords patients may use to find your practice. Use descriptions that match the language patients would use. Not only does that improve understanding, but it will also signal relevance during the rankings process.
• Choose the Correct Categories: Search engines will consider the category you select when ranking your practice. The primary category should reflect your main specialty. Meanwhile, secondary categories can encompass any sub-services relevant to your practice.
• Use High-Quality Photos: Publishing high-resolution photos goes a long way in healthcare digital marketing. Ensure that you include exterior shots that patients can use to identify your building, interior shots to establish trust and photos of your staff to enhance credibility.
• Create Virtual Tours: Consider creating virtual tours that showcase your property. Many patients find visiting a new practice daunting, and a virtual tour is a fantastic way to ease their worries. Additionally, tours can enhance user engagement and establish credibility.
• Enable Online Booking: Enable or promote online booking. Google's "Reserve with Google" feature connects with third-party scheduling software, allowing patients to request appointments directly on your profile. Online booking reduces conversion friction, potentially leading to an increase in appointment bookings.
• Add FAQs: Add a FAQs section to your GBP to address common patient questions and concerns. You can also use this FAQs section to incorporate more relevant keywords.
• Post Updates Regularly: Regular posting signals to Google that your profile is active and well-maintained. Use Google posts to keep patients engaged. Provide health tips, make posts about your practice's day-to-day and more. As always, maintain HIPAA compliance while applying all E-E-A-T requirements.
Local SEO for Doctors: Directory and Citation Management
It's not enough to complete a profile and hope for the best. Successful SEO for doctors also involves getting on as many directories as possible. You want others to mention and link to your practice. Citations help to build authority. The more websites that point visitors to your Google business profile and website, the more authoritative you become.
Citations also boost local pack rankings, drive referral traffic and strengthen overall patient trust.
Work to get your practice included in local and regional directories, including those maintained by your local chamber of commerce or state associations. Doing so will validate your local presence.
To strengthen your medical practice SEO efforts, you must also get your business on medical directories such as:
• Zocdoc
• Healthgrades
• Vitals
• WebMD
• RateMDs
• CareDash
• Doximity
Focus on directories that align with your specialty. For example, mental health practices will want to receive citations from GoodTherapy, Psychology Today and Alma. Meanwhile, dental clinics should have citations from the American Dental Association and DentalPlans.com.
Consider creating a master sheet for all citations to ensure consistency and accuracy. Consistency is paramount. In addition to ensuring that all names, numbers and addresses are the same, you should use matching language when describing specialties and credentials. Having a master sheet makes it that much easier. You can also utilize third-party tools that check consistency across directories. These tools can even check for missing links and help you make updates if information changes.
Healthcare Digital Marketing: Content That Converts Patients
Now, let's talk content. High-quality content is at the heart of medical practice SEO. The entire goal is to publish content that potential patients find helpful. The more valuable and authoritative your content is, the more it'll help drive organic traffic to your website.
Focus on evergreen content that's relevant to patient concerns. All content must be HIPAA-compliant to protect sensitive information. However, it must also be informative yet accessible.
One of the most challenging aspects of medical practice marketing is striking a balance between showcasing your practice's expertise and presenting information in a way that's easy for patients to understand. Most patients aren't well-versed in medical jargon. They're searching the web to learn more about the services you provide, so you must approach content creation from a patient's point of view. That means delivering content in a format that's easy to follow, information-rich and authoritative
Medical Website Optimization for Patient Education
The best way to approach healthcare SEO optimization from a content creation standpoint is to educate. Your website's content is not intended for other healthcare providers or trade organizations. It's for the everyday person concerned with their healthcare journey. Fortunately, many types of content can resonate with patients. Here's a quick breakdown of what you can publish on your site to build authority, earn trust and convert visitors.
• Condition and Symptom Guides: Google reportedly receives 70,000 health-related searches a minute, and many revolve around specific symptoms and conditions. Symptom guides offer incredible value, providing answers and information on subjects that patients are actively seeking.
• Educational Blogs: Educational topics are another heavy hitter. As a medical practice, you can utilize your expertise to provide helpful tips or "what to expect" guides on various conditions, treatments and other relevant topics.
• Treatment Comparison Pages: Healthcare providers can address health concerns in many ways, and many patients want to learn more about their options. Content that explores the differences and similarities of treatments offers exceptional value.
• Procedure Pages: Many patients conduct research before a scheduled procedure. As part of your medical practice SEO efforts, you can create pages dedicated to detailing how the procedures your practice performs work.
• How-To Guides: How-to guides are an excellent way to earn trust. You can publish guides on how to manage conditions, prepare for treatment and handle post-procedure follow-up care, among other topics.
• Patient Stories: Patient stories and testimonials provide social proof about your practice's capabilities. They're also a great way to demonstrate how your practice approaches things differently from competitors, such as larger health systems.
When creating this content, always consider what patients are looking for and take steps to link to other pages on your site. Adding sections that cover frequently asked questions or "what to expect" goes a long way in building trust and authority while proving your expertise. Content that directly addresses a visitor's concerns can help you attract new patients while enhancing your site's search engine rankings.
HIPAA-Compliant SEO Content Creation
Search engines like Google scrutinize medical content, and for good reason. There are many legal repercussions for violating HIPAA or spreading misinformation.
Always maintain HIPAA compliance. Don't include any patient-identifiable information. Avoid using full names or detailed medical histories in your content. Instead, keep your content more generalized. The best approach is to provide general condition information without referring to specific people.
If discussing real-world cases, anonymize the data to protect your patients and practice. When gathering testimonials to publish, get explicit consent from your patients and ensure statements don't include any protected information.
Beyond HIPAA compliance, there are also several legal implications to consider. SEO for medical practices can easily fall into risky territory. Avoid making any strong claims, promises or guarantees. For example, guaranteeing positive outcomes or claiming to be the "best" provider in the area could constitute false advertising. Steer clear of any unsubstantiated claims or overstated income.
To maintain the factual accuracy of your website, always clearly identify the author's credentials and provide links to authoritative, peer-reviewed studies. It's also wise to include disclaimers where appropriate. Your content is intended solely for informational and marketing purposes. Therefore, you can't provide medical advice. Providing a disclaimer that says as such will protect your practice from liability.
Advanced Medical Practice SEO: Technical Optimization
The quality of your content matters when developing strategies for high-impact medical practice marketing and SEO enhancements. However, success hinges on more than just the content you produce. Beyond on-page SEO, you must also invest in technical SEO.
We already covered some pivotal technical details that could improve your website. These include optimizing your website's loading speed, enhancing security and ensuring your site is accessible on mobile devices. Technical SEO can influence your rankings. Search engines like Google won't rank clunky websites with poor performance. Therefore, investing in improvements to ensure your site offers a smooth experience for visitors goes a long way.
If your website also offers online booking features, ensure you get an appropriate SSL certificate. An encryption security protocol will protect patient information.
Transform Your Medical Practice with Professional SEO Implementation
Medical practice SEO isn't something you can afford to ignore. Modern patients are more involved in their healthcare than ever before, taking an active role in finding providers that meet their distinct needs and preferences. Thanks to the Internet, patients can receive care on their own terms. As a medical practice, your success hinges on your ability to reach patients where they are. Healthcare SEO optimization helps you achieve this, but it can be a significant undertaking.
Medical SEO strategies are complex, and expertise matters. Successful SEO for medical practices can pave the way to stronger online visibility, more appointment bookings and sustained growth. It provides a greater ROI than traditional medical practice marketing techniques and can even provide your practice with a competitive advantage over larger health systems with bigger advertising budgets. But to realize those benefits and more, you need professional medical website optimization and expert medical practice SEO implementation.
Put your practice on a path to success while saving time, maximizing your ROI and achieving measurable, sustainable growth that counts. Give your practice what it needs to compete with the big dogs. Reach out to Fuse today to schedule your medical practice SEO consultation and see firsthand how the right strategies can help you book more patients and boost your bottom line.
Preparing for AI-Powered Search: Future-Proofing Your Medical Practice
As AI-powered search tools become more common, forward-thinking medical practices are starting to optimize for these new technologies. While traditional SEO remains the foundation, preparing for AI search can give your practice an early advantage.
AI assistants and tools like ChatGPT are increasingly used for health-related questions, and Google's AI Overviews now appear for many medical searches. To optimize for these platforms, focus on creating content that AI can easily understand and cite. Use clear, structured formatting with descriptive headings and bullet points. Implement FAQ schema markup to help AI assistants find and present your information accurately.
The key is making your content conversational and comprehensive. When patients ask AI tools questions about symptoms or treatments, you want your practice's information to be the source that gets referenced. This means writing in natural language that matches how people actually speak and ask questions, not just how they type into search engines.




.avif)
.avif)
.avif)

.avif)
.avif)


