How to Create a 5-Star Digital Patient Intake Experience That Transforms Your Practice
In most practices today, you almost expect to see the same scene: A crowded waiting room full of patients with front-desk staff scrambling to enter data from a stack of clipboards. Sound familiar? An outdated patient onboarding process is a recipe for disaster. Paper forms and old-school processes lead to lengthy wait times, a high risk of data entry errors, frustrated patients and overworked staff.
Did you know that patients spend, on average, 15 to 20 minutes completing forms in a waiting room? If they're a new patient, they often spend even longer. That time adds up, putting a significant burden on your administrative staff while starting patient visits off with a frustrating experience.
It doesn't have to be that way. A streamlined digital patient intake process can address those common pain points and more, giving your practice a competitive advantage while simplifying workflows across the board. Recent surveys show that 73 percent of patients prefer digital intake options. Digital solutions make things easier for everyone, freeing up your staff to focus on delivering top-quality patient care while making visits less stressful for patients. Digital approaches also significantly reduce data entry errors that could cause chaos downstream.
Why Traditional Patient Registration Systems Are Failing Your Practice
While the pandemic certainly accelerated the adoption of digital intake processes and online patient portals, many clinics still use paper forms. One survey suggested that a significant number of practices still use paper processes, and a whopping 88 percent of hospitals rely on manual data entry for patient intake. Those outdated processes hinder medical practice in numerous ways.
• Clipboard Management: No one likes dealing with stacks of bulky clipboards. Not only do they waste valuable space, but staff must keep track of which patients have clipboards and which have already submitted forms.
• Illegible Handwriting: Hard-to-read handwriting can be a nightmare. Staff must spend time trying to decipher illegible writing and correcting inputs.
• Duplicate Data: Without automated patient registration, teams must manually input data into electronic systems or match information across records. That workflow creates a high risk of duplicate data entries. One study found that duplicate records can cost practices up to $1,000 to correct duplicated data and records.
• Manual Error: With manual data entry comes a risk of human error. Even the most vigilant administrators can make mistakes, but they can be costly. Up to 86 percent of all healthcare mistakes are administrative and a direct result of inaccurate data entry.
• Insurance Verification Delays: Errors during registration and insurance verification are reportedly the cause of 25 percent of all insurance claims denials. With incorrect information, insurance eligibility checks take longer. Practices also waste valuable time and effort in identifying errors, repeating verification checks and reworking claims forms.
• HIPAA Compliance Risks: Paper forms are more challenging to secure. They're more vulnerable to theft, misfiling and unauthorized access, presenting risks of HIPAA violations.
On top of those concerns, paper forms create a less-than-stellar patient experience. Most clinics ask patients to arrive up to 20 minutes before an appointment, all to complete paper forms. It's a frustrating process made worse by the fact that most of the information provided is redundant. In one survey, 83 percent of respondents said they had to provide duplicate information.
These issues all compound to affect your practice's bottom line. A poor patient experience actively harms your reputation. Furthermore, outdated processes that are prone to human errors can negatively impact collection rates, delay reimbursements and create additional administrative work, ultimately leading to staff burnout.
The Complete Digital Patient Intake Journey: From First Contact to Treatment
In 2025 and beyond, patients expect a seamless digital experience. Patient experience optimization should be a top priority, but what does a patient's digital journey look like? The ideal patient experience begins before their visit, featuring online support and automated patient registration.
• Online Appointment Booking: Patients should be able to schedule appointments digitally without having to call your office. A reported 67 percent of patients prefer online booking. Allowing people to choose a date and time that works for them can help reduce no-shows. Send automated reminders to prevent last-minute cancellations.
• Pre-Visit Patient Intake Software: Why spend time in the office completing forms when you can streamline patient intake by having them do it at home? With patient intake software, your practice can encourage individuals to complete intake forms, consent documents, medical history forms and more before their visit. Digital healthcare intake management and patient registration systems save valuable time and can reduce errors associated with manual data entry.
• Insurance Verification: Real-time insurance verification ensures that your practice and your patients understand coverage before a visit. Patients will have a better understanding of their insurance eligibility, and practices like yours can address any issues before rendering treatment or submitting claims.
• Cost Estimates: In addition to verifying insurance, your practice can provide automated digital cost estimates. Doing so gives patients a better understanding of their financial responsibilities. It reduces anxiety over clinic visits, helps them prepare for visits and can help increase collection rates.
• Visit Check-In Upon arrival, self-serve kiosks or tablets allow patients to check in quickly and effectively. Digital systems save time, eliminate the need for traditional paperwork and prevent lengthy wait times.
Essential Features Your Intake Software Must Have
Patient intake software can transform your practice, improving healthcare intake management strategies while saving everyone time and effort. The best software will streamline workflows and help improve your revenue cycles. There are many features to look for, but the following are non-negotiables your software needs to have.
• HIPAA Compliance: HIPAA compliance should be standard. The software you use should protect all digital intake forms, safeguarding protected health information (PHI) to meet federal regulations. Look for features like strong encryption and user authorization.
• Smooth EHR Integration: You want your patient onboarding process to be as smooth and error-free as possible. That requires smooth EHR integration. Integration with existing EHRs ensures that data flows between systems without a hitch, preventing duplicate data and errors.
• Mobile Optimization: An estimated 55 percent of patients in the U.S. prefer using mobile devices for managing healthcare appointments and records. Patients should have the ability to complete digital intake forms on smartphones or tablets.
• User-Friendly Interfaces: Intuitive interfaces and guided workflows benefit both staff and patients. Clunky experiences only add frustration, impacting abandonment rates and creating more incomplete forms your staff needs to fix.
• Customizable Forms: Digital patient intake software should allow you to create and customize forms to meet your practice's needs. That includes customizing forms based on your specialty and branding.
• Insurance Verification Capabilities: Real-time insurance verification features check eligibility in minutes, eliminating manual work and delays while reducing the risk of errors. Completing verification processes before a patient's visit will save time and ensure timely care.
• E-Signature Support: Software needs to support e-signatures. Without it, you'll still rely on paper forms. E-signatures can streamline consent processes.
• Photo Capabilities: Photo capture features can enhance patient records and help staff verify identities.
•Technical Considerations: All software that helps improve healthcare intake management needs strong security protocols, including robust encryption and access control. However, it's also wise to seek solutions with API capabilities. APIs help with scalability and integration.
HIPAA-Compliant Digital Intake Forms That Patients Actually Complete
It's one thing to make intake forms available digitally. However, it's another to design forms that patients will actually complete. There's an art to developing intuitive, easy-to-understand digital intake forms. Failing to consider the patient experience when completing these forms can result in high abandonment rates and even more frustration.
First, ensure that forms are accessible on the devices that patients want to use. Take a mobile-first approach. Ensure that all forms are optimized for mobile devices and support features like touch input. Because mobile screens are comparatively small, keep scrolling to a minimum and ensure that all buttons and text are large enough for optimal visibility.
Forms themselves need to be concise and logically organized. The best approach is to use progressive disclosure. Only show questions that are relevant to patients in the moment. For example, you don't need to ask patients questions about insurance if they plan to pay out of pocket. Therefore, you'd only unveil insurance-based questions once patients answer "yes" to a question like "Do you have insurance?"
Questions should make sense and flow from one to the other. Generally, it's best to ask for personal details before moving on to insurance, medical histories and consent. To make things more predictable, implement a visual progress bar.
When completing more complex forms, the key is to simplify the process. Throwing tons of confusing questions at patients will only increase abandonment rates. You want to break things down into manageable chunks. Provide clear queries and guidance. Your digital intake forms can also offer inline tips to help patients understand what you're asking. Intuitively guide patients from one section to the next until they reach completion.
Thoughtful UX design goes a long way. Put yourself in your patients' shoes and see how it feels to complete forms yourself. Fine-tune design elements and simplify things as much as possible. When done right, the process will be a cinch.
Automated Patient Registration Features That Save Hours Daily
If you're looking to streamline patient intake as much as possible, automation is the way to go. Fortunately, patient intake software can have automated features that make the lives of your staff and patients significantly easier. Here are a few to look for.
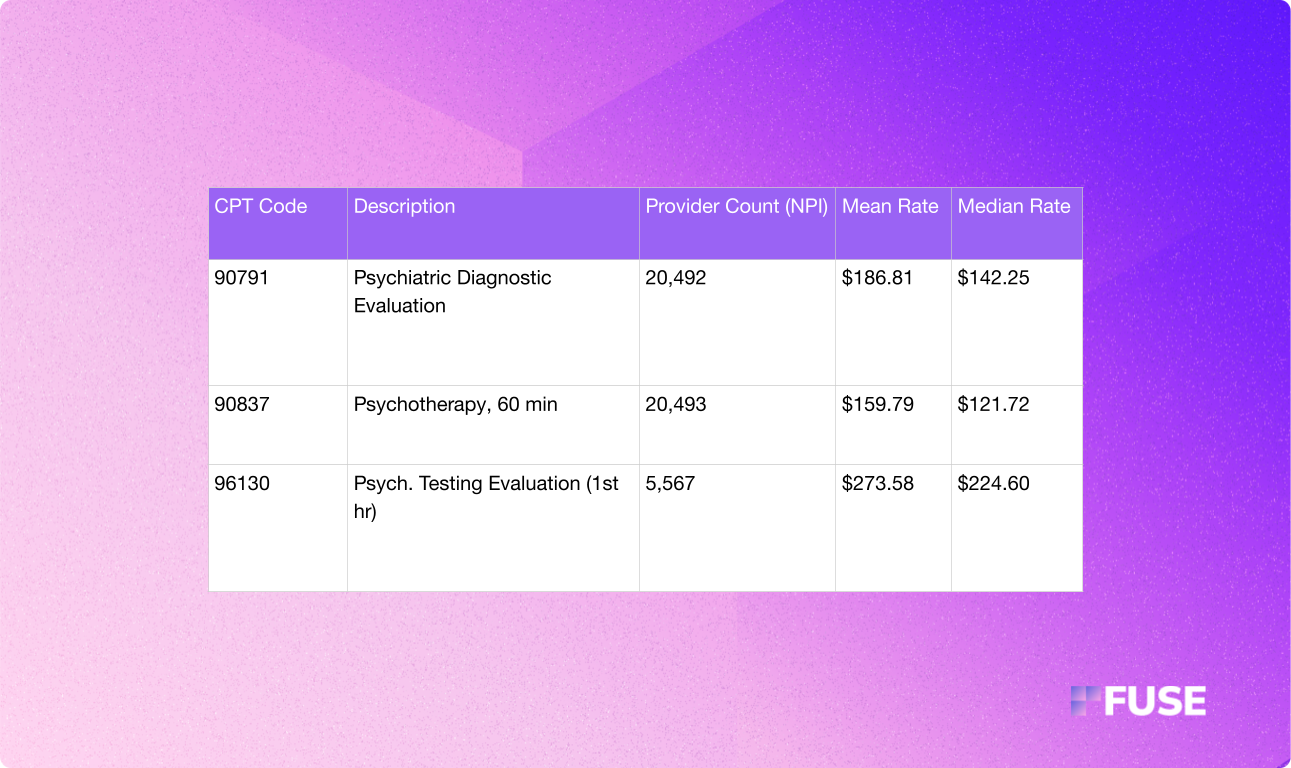
• Insurance Verification and Eligibility Checks: Automated insurance and eligibility checks can save hours of manual work. You can verify insurance coverage in real-time. Software that performs checks on the CPT code level can even provide more information bout preauthorization requirements, limits and other coverage specifics. Manual insurance verification takes, on average, 12 minutes per patient, assuming you don't need to make a phone call to a payer. However, with automated real-time verification, you can do it in just a few minutes.
• Demographic Updates: Automated software helps practices ensure accurate and updated patient information. Integration with practice management systems and EHRs can streamline demographic information capture, preventing duplications and errors.
• Appointment Confirmations: Systems that send out automatic reminders and confirmations can dramatically reduce the rate of cancellations and no-shows. Furthermore, you free up your staff to focus more on patient-centered care rather than spending hours on the phone.
Overall, automated features can have a positive ripple effect on your practice and its revenue cycle. These features virtually eliminate the need for hours of manual data entry. Additionally, they help reduce errors that often require hours to correct. With seamless integration with existing practice management systems, automated tools can reduce administrative workload by as much as 30 percent. According to the 2024 CAQH Index, automated workflows have the potential to save the entire healthcare industry around $20 billion.
Healthcare Intake Management Systems That Scale With Your Practice
As practices expand, healthcare intake management systems must grow, too. Scalability is something your practice needs to consider when choosing the right digital solutions and tools. It's essential to maintain operational efficiency while striving for long-term success.
Some key features and scalable capabilities to consider include multi-site support, customized options tailored to different specialties and robust analytics.
Multi-site support offers centralized management capabilities, enabling administrators to deliver consistent experiences across multiple locations. Having the ability to manage several locations can reduce administrative work while maintaining compliance and high standards across the board.
Customized options ensure your software can accommodate the unique needs of different specialties. Scalable solutions will offer custom frameworks, workflows and consent forms tailored to each specialty.
Finally, strong reporting capabilities and analytics help practices gain actionable insights when it matters. Easy-to-read dashboards, comprehensive reports and trackable KPIs make it easy to identify opportunities for improvement on your journey to growth and enhanced efficiency.
Growing your practice can be overwhelming, and there are many scalability concerns to address. To choose the right software for your needs, turn to options that offer enterprise-level features. API integrations, advanced user permissions and authorizations, clear audit trails and in-depth reporting give you all the tools to grow. Additionally, these features can help create a roadmap for sustainable expansion, paving the way for growth without the associated growing pains.
How to Streamline Patient Intake Without Overwhelming Your Staff
Making the switch to more efficient patient registration systems can be overwhelming for your staff. There are many benefits on the horizon, but you can only reap those rewards if you can manage the transition without issue.
Start by communicating with your staff. You want to explain how the change can benefit your team, highlighting how automation will support roles while streamlining workflows. Gather feedback early and listen to your staff. Being receptive and transparent can increase buy-in.
From there, you should map out existing intake processes. Identify the pain points your staff encounters and see how new solutions and tools can alleviate them. Demonstrate those improvements to your team to emphasize further the positive impact this transition can have.
Like any other major workplace change, it's best to implement new solutions in phases. For example, you can begin by allowing patients to schedule appointments online. Then, you can move towards making forms available for patients to complete before their visit. Once you have successfully implemented those changes, you can move on to automated real-time insurance verification and more complex tasks. Take things slow, allow staff to familiarize themselves with their new workflows and continually accept feedback.
It's also wise to still make paper forms available during the early stages of your transition. Doing so will accommodate patients who prefer them and can ease the transition to digital workflows for your staff.
As always, provide hands-on training and support. Change can be difficult for staff members who are accustomed to doing things one way, even if those old methods are less efficient. Provide guidance when necessary, resolve issues promptly and make support easily accessible to all.
Measuring Success: ROI Metrics That Prove Your Investment in Digital Intake
Investing in tools that offer automated patient registration and streamline intake processes is a significant move. However, it's an investment that can pay off. To prove the value of new initiatives and tech implementation, you need to track several KPIs.
Practices can present these metrics in executive summaries and ROI reports to prove the efficiency of patient intake software. Furthermore, tracking the right KPIs can help you optimize your strategies. Using dashboards to track key metrics makes identifying opportunities for improvement easier than ever, leading to enhanced medical practice efficiency and patient experience optimization that you can quantify.
Core KPIs you should monitor include:
• Wait Times: Reduced wait times can show real value in the tools you use to improve the patient registration process. Currently, the average wait time for patients is 20 minutes. However, digital intake forms and automation can cut that in
• Patient Satisfaction Scores: Patient satisfaction scores can easily highlight the impact of tech investments. Roughly 73 percent of patients prefer digital intake processes, significantly improving patient satisfaction from the start.
• Staff Overtime: Substantial administrative burden caused by outdated manual processes can lead to hours of staff overtime. Tracking this metric will highlight how much patient intake software reduces workload.
• Revenue Cycles: Faster revenue cycles are always a plus. Because digital intake software and automation save time while reducing errors, you can track this metric to show how changes help your practice beat the industry benchmark of 30 to 50 days in accounts receivable.
• No-Show Rates: The average no-show rate is between 5 and 7 percent, but some specialty clinics can experience rates as high as 30 percent. With online appointment-setting and automated reminders, the right software can help you see marked improvements in this area.
Ready to Transform Your Patient Experience?
The patient experience begins long before a visit to your clinic. Practices that prioritize highly efficient digital patient intake processes gain a significant advantage. Modern patients expect digital convenience and mobile-friendly interactions. Adopting patient intake software early on to meet the demands and expectations of patients can give your practice a competitive edge, positioning it as a forward-facing practice that focuses on creating a stellar experience for patients.
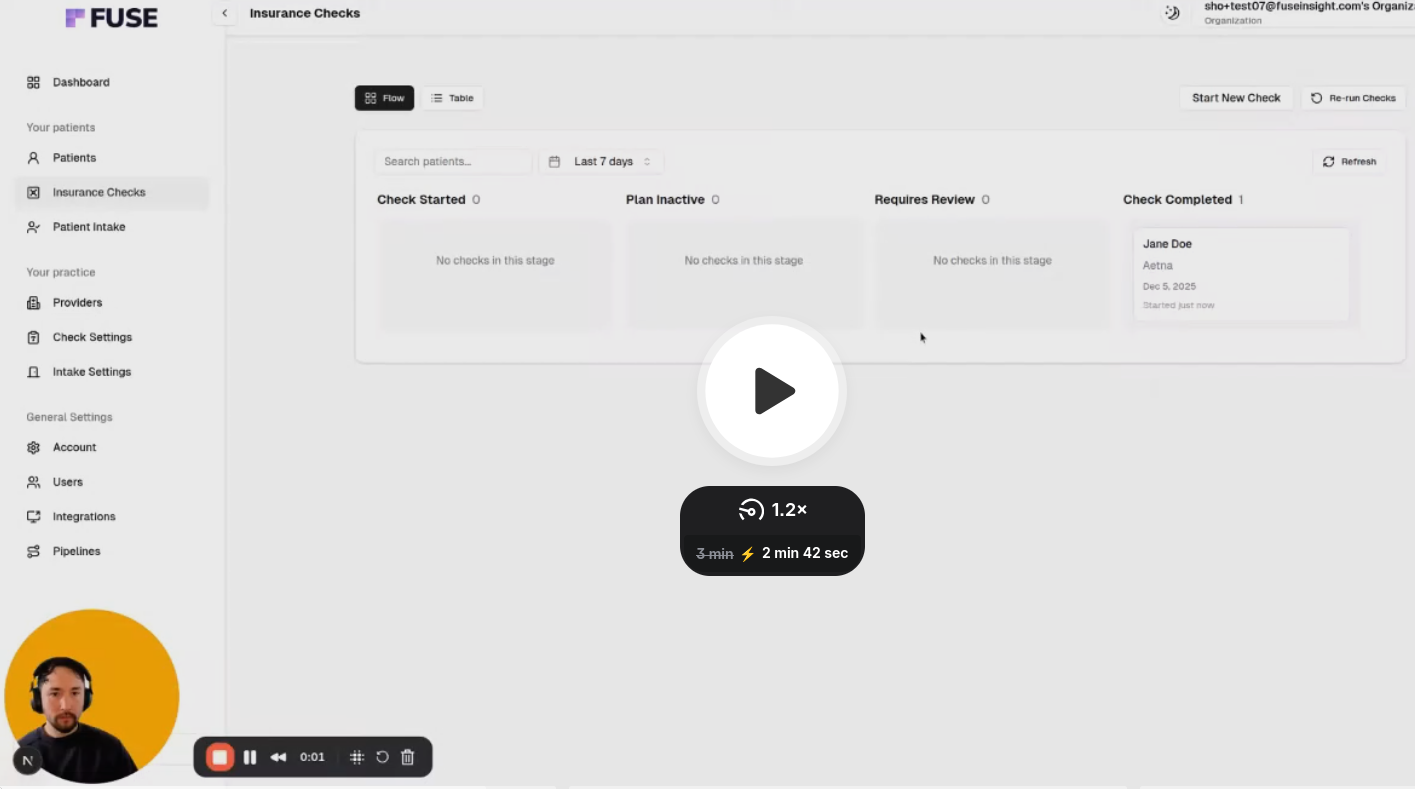
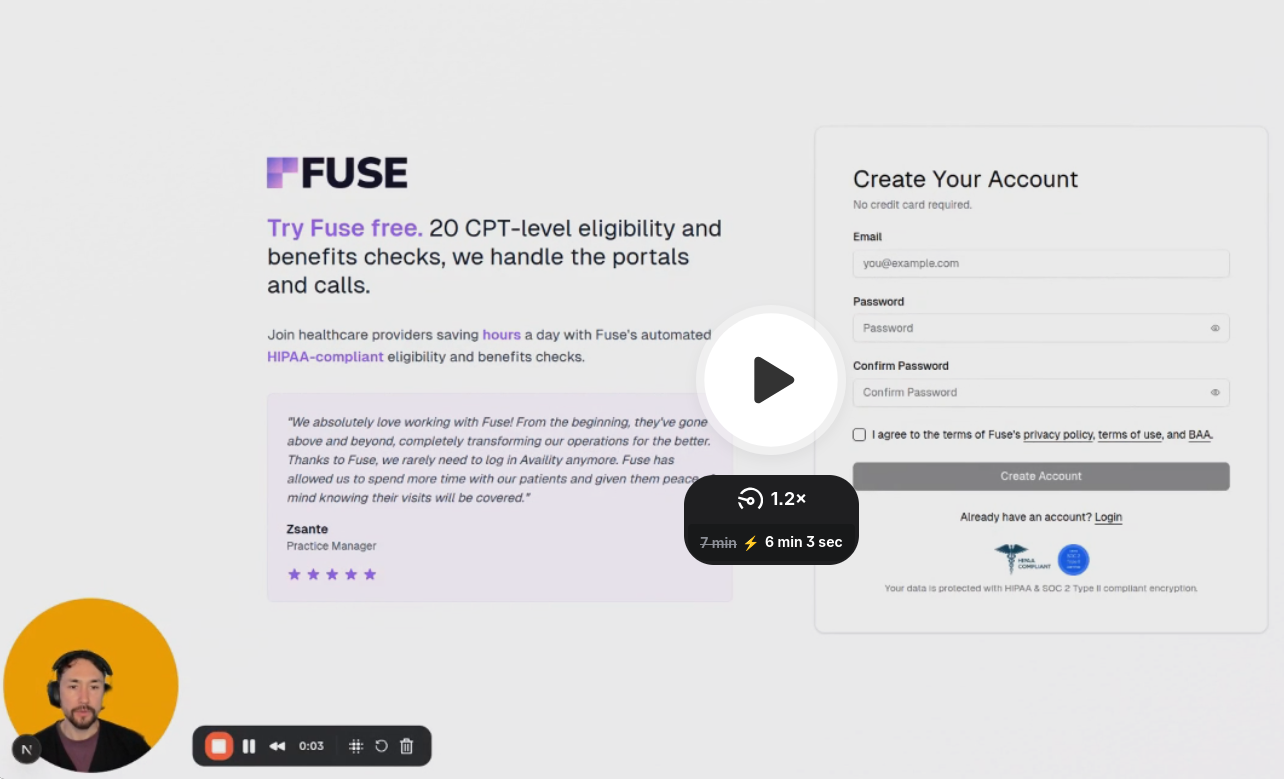
With more and more practices leveraging technology to streamline patient intake and other administrative workflows, you can't afford to hold back. Fortunately, Fuse is here to help you leverage automation to save time and maximize revenue.
Fuse is a state-of-the-art software solution that automates patient intake, CPT code-level insurance verification and cost estimates. With Fuse, you can transform your practice in numerous ways and achieve a rapid return on your investment. With implementation support and more revolutionary features to come, you have nothing to lose and everything to gain.
Schedule your Fuse demo today to see firsthand how it can help you create that five-star experience patients want.
FAQs
Software solutions that facilitate digital patient intake and automated patient registration must be HIPAA compliant. They need end-to-end encryption, safe data storage and user access controls with strict authorization capabilities to keep all PHI safe.
Implementation time can take anywhere from a few days to several months for larger health systems. Transitioning to a more robust patient registration system in phases may add additional time. Options like Fuse offer implementation support every step of the way.
Patient intake software integrates directly with EHR systems, allowing for seamless data transfer between the two. Successful integration reduces duplicate data entries and errors, thereby improving accuracy and efficiency. While integration capabilities vary, the best solutions will create a strong connection for effortless data sharing.
While most patients want digital intake forms, that's not true for everyone. To help those who aren't particularly comfortable or tech savvy, practices can still offer paper forms or complete registration via staff-assisted data entry processes.




.avif)
.avif)
.avif)

.avif)
.avif)


