5 Critical Patient Intake Mistakes That Cost Healthcare Providers Time and Money
In the United States, healthcare providers spend roughly 30 percent of their operating budgets on administrative activities alone. Recent surveys suggest that the average medical intake process costs up to $23 per patient. Multiply that by thousands of patients annually, and inefficient medical intake workflows are costing practices big. However, what's more worrying is how outdated processes are resulting in widespread patient intake mistakes.
Simple mistakes, such as inaccurate data entry and incomplete information, can create unnecessary delays and preventable barriers to successful patient care. According to the World Health Organization, up to half of all medical errors in primary care are a result of administrative missteps. Some research suggests that 30 percent of medical claim denials are due to imprecise patient data.
Not only do healthcare provider intake errors cost providers time and money to correct, but they can also impact patient safety. Fortunately, these mistakes are entirely avoidable with the right system and ample training. Keep reading to learn more about the five most common mistakes made during the medical intake process and how your practice can avoid them.
Why Patient Intake Accuracy Matters More Than Ever for Healthcare Providers
Modern healthcare relies heavily on data, and regulatory compliance requirements are putting a heavier burden on practices and providers. The HITECH Act expanded security regulations under HIPAA, creating more compliance requirements for electronic health record intake systems. These new regulations aim to enhance data quality, minimize patient registration errors and improve patient safety. Providers must be more vigilant about avoiding mistakes to comply with regulatory standards while also ensuring patient safety.
Patient intake mistakes compromise safety in many ways. Incorrect data can lead to misdiagnoses, improper treatments, medication errors and delays in care. These mistakes can affect the quality of care that patients receive, potentially having life-changing impacts. But that's not all.
Because healthcare intake forms directly affect billing, insurance claims and reimbursements, mistakes can result in lost revenue. Claim denials reportedly cost hospitals and health systems nearly $20 billion a year! With a significant percentage of denials being caused by data errors, the need for improved workflows and rock-solid patient intake software is at an all-time high.
Mistake #1: Incomplete Medical History Collection
One of the most common healthcare provider intake errors that affects patient care and safety is incomplete data about an individual's medical history. Rushed medical intake workflows leave little time for patients and administrators to paint the whole picture. While many focus solely on basic identification data and insurance information, providers need to understand a patient's medical history to provide efficient care.
Without that critical information, providers can make grave mistakes when diagnosing a patient's condition. That lack of data can also lead to incomplete or potentially harmful treatment plans. For instance, some common bits of information that rushed intake processes miss include allergies, drug sensitivities and psychological health concerns. Without that information, providers can inadvertently develop treatment plans that actively harm patients.
Best Practices for Comprehensive Medical History Forms
Healthcare intake forms and processes need to be comprehensive. No matter how rushed practices are, there are several sections your medical history forms should never skip. These include:
• Allergies
• Medications
• Previous surgeries
• Family histories
• Chronic conditions
• Immunization status
These details all help healthcare providers treat patients successfully. Medication reconciliation and information about allergies will inform providers about what to avoid. Meanwhile, family medical histories can help providers understand a patient's unique risk factors.
Urging patients to provide complete information without skipping sections can be challenging, especially in a rushed environment. Patient intake best practices recommend giving individuals ample time and flexibility. Provide options on how patients can provide necessary data, including self-administered forms or verbal disclosure. Administration should communicate the importance of providing this critical information, all while remaining sensitive to a patient's need for privacy.
How Technology Improves Healthcare Intake Forms Accuracy
Technology can transform your entire medical intake process. Patient intake software digitizes the process, helping prevent errors and omissions that could impact care. Digital forms with validation are an effective way to ensure that the information gathered is accurate. User-friendly processes force patients to double-check the information provided, dramatically reducing errors. When integrated with EHR systems, digital forms make a difference.
Features like automated reminders can also prevent incomplete sections, encouraging patients to provide all relevant information about their medical history, medications, allergies and other pertinent details.
There are countless benefits to implementing technology into your patient intake workflow. However, the most significant is that patients can provide critical information on their own terms. Patients can complete forms at home before their visit, rather than spending 20 minutes rushing through them in the office.
Mistake #2: Poor Insurance Verification and Patient Registration
Insurance errors are another administrative headache that costs providers billions annually. The financial impact is monumental. Patient registration errors often lead to denied claims, which impact both providers and patients. Insurers that offer plans on the Health Insurance Marketplace deny nearly 20 percent of in-network claims and 37 percent of out-of-network claims, and a significant percentage of those denials are due to poor insurance verification. Almost 27 percent are a product of eligibility issues.
Each processing error reportedly costs providers up to $125 to identify and correct, with claims adjudication costing providers over $25 billion annually. On top of all that, patient billing disputes significantly increase administrative costs.
Insurance verification should be a top priority during the patient intake process. Verification should occur before a patient even steps foot in the office. By verifying insurance information and eligibility before a visit, practices can avoid denied claims and ensure patients have coverage before rendering treatment. Waiting until after a patient's visit will only increase the risk of denials and disputes.
Streamlining Patient Registration Process for Better Outcomes
Many practices use patient intake software, but they often fail to complete adequate insurance verification. While many promise to check eligibility, they don't do so accurately, forcing many practices to turn those features off entirely.
Patient intake best practices involve step-by-step verification processes. Software should effectively perform real-time eligibility checks, ensuring everything is in order before a patient's office visit. Patient intake software should also collect backup insurance documentation to prevent delays in care and over-complicated claims processing.
The best software utilizes AI to automate these tasks, freeing up staff and streamlining the registration process from the outset.
Mistake #3: Inadequate Staff Training on Medical Intake Workflow
Undertrained staff can create bottlenecks in your medical intake processes. Administrative teams need to operate like a well-oiled machine. Otherwise, the process can be a nightmare for healthcare providers and patients alike.
As bottlenecks develop, staff will have no choice but to rush through the process. The result is an increase in data entry errors and a lack of consistency. Training gaps in HIPAA compliance may also elevate your risk of data breaches, penalties and reputational damage.
A lack of training for administrative personnel can harm your practice in countless ways. It has a ripple effect, compounding patient frustration and leading to more patient intake mistakes that require time and money to correct. Furthermore, neglecting comprehensive training can lead to high turnover rates, which in turn add further confusion and chaos.
Essential Training Components for Patient Intake Teams
Every member of your administrative team needs thorough training. Successful patient registration processes require strong verbal communication skills, active listening and a deep understanding of how to avoid potential errors. Teams also need HIPAA compliance training and education about insurance verification processes.
Training can be time-intensive and costly. Furthermore, even with ongoing efforts to improve skills and workflows, errors are still possible. Practices like yours should consider automation. Patient intake software that can handle more complex administrative tasks will improve efficiency, reduce manual errors and allow administrative teams to focus on serving patients in other ways.
Mistake #4: Lack of Quality Control and Error Tracking
Combating patient intake mistakes is a constant battle for practices. One study found that over 20 percent of patients identified errors in their own medical records. That's just including patient-reported issues. Those that go unnoticed until they create patient care or insurance processing issues are likely far higher.
Many patient intake processes lack quality control and error tracking. As a result, mistakes slip through the cracks. Successful quality control requires a multipronged approach. However, automation can do much of the heavy lifting, removing the burden on administrative staff. Modern patient intake software can automate error tracking entirely; practices need to take advantage of these capabilities.
Implementing Effective Intake Quality Assurance Programs
Quality assurance programs and automation can make a world of difference. Successful implementation is about understanding the types of errors that impact your practice and developing strategies to avoid them. Error tracking systems can help identify issues early on, allowing providers and administrators to address them before they impact patient care. Meanwhile, regular audits can scrutinize current medical intake workflows and highlight areas that require improvement.
Quality control is a data-intensive process, and there are many metrics that practices should track to monitor potential patient intake errors. Data should be the driving force for change. Audits can highlight challenges, enabling providers to easily identify training needs and system improvements that can foster positive change. Some key metrics to track include:
• Patient data accuracy rates
• Claim denials
• Correction time
• Missing form rates
• Missing identification data
• Audit failure rates
Mistake #5: Outdated or Inefficient Patient Intake Software Systems
Inadequate software is a bigger source of patient registration errors than most providers realize. Technology in the healthcare space is nothing new. Practices have utilized software to streamline patient intake for decades. However, legacy systems aren't capable of keeping up with modern demand, and many older software tools create more work than necessary.
Dated software can lead to more errors, frustrating both staff and patients. Inefficient workflows and inoperability issues can create more problems than the software claims to solve.
Poor EHR integration is a common problem with older software programs. Inconsistent data formats and a general lack of data standards often lead to omissions and errors. Weak integration can also create manual data entry problems. Older patient intake software may even lack robust security protocols, creating vulnerabilities and concerns regarding HIPAA compliance.
Legacy systems are a byproduct of a time when automation was lean. As a result, many intake providers simply don't have the capabilities that modern healthcare providers need. For example, many don't perform insurance eligibility checks and lack any automation features that can truly streamline your medical intake workflow. Some don't even have features that allow you to customize forms to match your practice's branding.
Key Features to Look for in Modern Healthcare Intake Solutions
Upgrading your patient intake software can take your workflow into the 21st century, helping your practice work more efficiently while avoiding errors that can negatively impact your business and the patient experience. While many providers hesitate to make such a significant change, investing in new patient intake solutions can deliver a high ROI.
The right software can greatly reduce administrative costs and lower insurance claim denial rates. Those benefits create a less stressful experience for patients, ultimately improving your practice's reputation and bottom line. While implementing new software can be daunting, the investment is well worth it. Depending on the size of your practice, implementation can take as little as a few weeks. You can get up and running in no time, moving toward a more efficient and error-free future.
So, what features should providers look for in patient intake software?
•Smooth EHR Integration: Proper EHR integration can save your staff time and eliminate the need for manual data entry. With integration, software can automatically populate a patient's EHR with data.
•Automation: Automated workflows simplify the medical intake process. Automation can create a digital experience that helps your practice capture all relevant data while reducing your administrative burden.
•Real-Time Insurance Verification: Real-time verification eliminates delays, errors and denials. You can verify insurance eligibility before administering care, all without the error-prone manual processes.
•Mobile Compatibility: Mobile compatibility allows patients to complete forms anytime, anywhere. Ditch paper forms and give patients more freedom to provide the information your practice needs.
•Analytics and Reporting: In-depth analytics and comprehensive reporting help you track errors and highlight inefficiencies that could impact your practice.
Transform Your Patient Intake Process with Proven Solutions
Patient intake mistakes don't have to cost your practice. Administrative costs are already at an all-time high for providers like you. Simple errors during the medical intake process create additional costs and delays, sacrificing the patient experience while putting their safety at risk.
The mistakes we mentioned are entirely avoidable. All it takes is the right patient intake systems and proper staff training. Fixing these mistakes with an end-to-end patient intake solution can lead to lower administrative costs, fewer error-caused claim delays and far better patient outcomes.
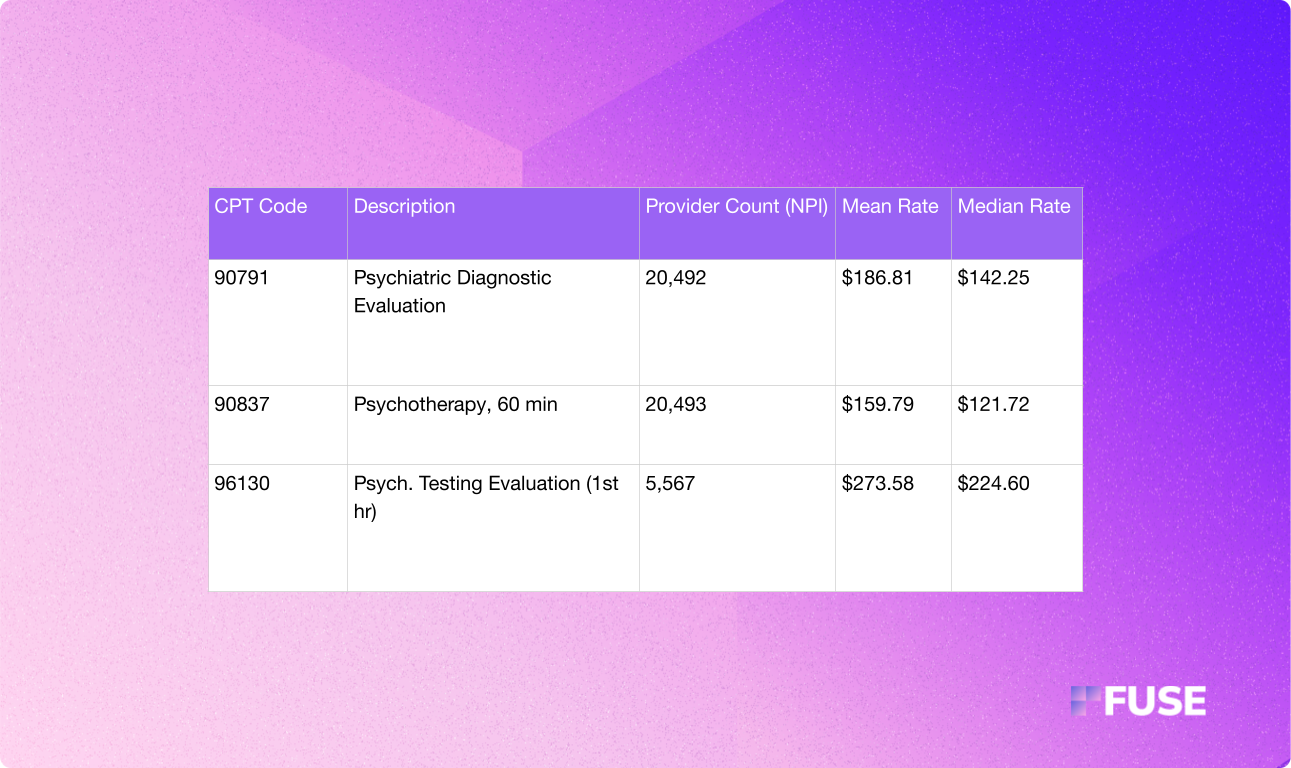
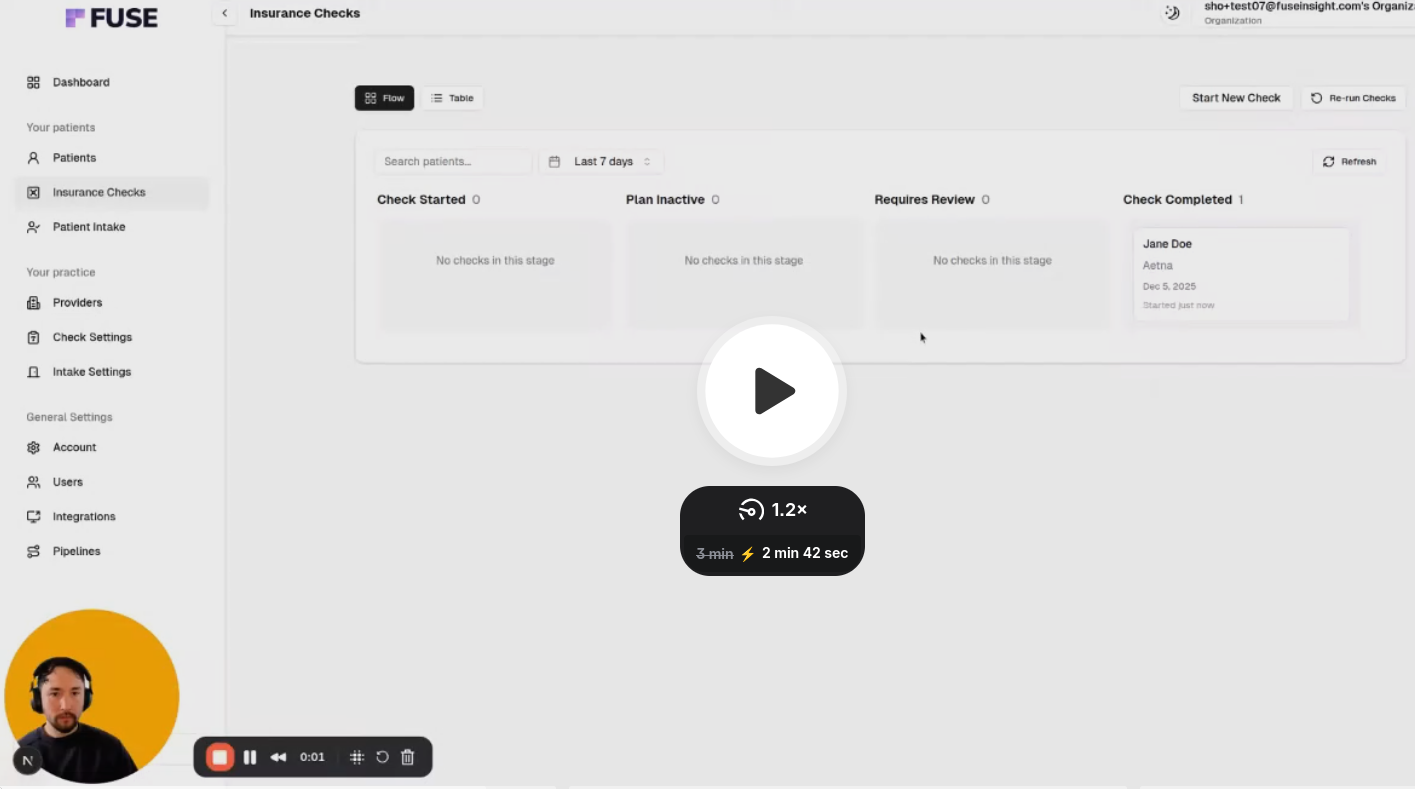
Fuse offers complete healthcare automation, streamlining the patient intake process while performing CPT code-level insurance verification. Prevent errors, eliminate the stresses of complicated intake processes and free up time to allow your team to focus on patient care. Schedule your Fuse demo today to learn more and see firsthand how an automated medical intake process can benefit your practice.




.avif)
.avif)
.avif)

.avif)
.avif)


