Streamline Your Revenue Cycle with Frontend Healthcare Automation
Manual revenue cycle processes slow everything down before a claim is ever submitted. Incomplete patient intake, missing insurance details, and rushed eligibility checks create bottlenecks that ripple from registration through billing and payment. By the time denials appear, the real problem has already happened upstream.
Fuse focuses on automating the front end of the revenue cycle, where most preventable issues start. We automate patient intake, insurance verification at the CPT code level, payer portal checks, direct payer calls, and fee estimates so your team doesn’t have to. The result is fewer downstream problems and more time for staff to focus on patients instead of administrative work.
Patient Trust
Streamlined RCM for eligibility and benefits checks leads to accurate patient cost estimates, better collections and an improved experience. Offer price transparency and reduce overhead with automation powered by Fuse.
Automated Patient Intake That Captures Every Detail
Patient intake is where accuracy matters most, but rushed forms and manual data entry often lead to missing insurance details and downstream billing issues. Fuse replaces paper and disconnected workflows with HIPAA-compliant digital intake that captures insurance and required forms upfront, eliminating rework and speeding up the front end.
.avif)
Real-Time Insurance Verification Without the Hold Music
Insurance verification wastes staff time as they jump between payer portals, phone calls, and spreadsheets just to confirm eligibility. Fuse automates this by checking payer portals, placing payer calls when needed, and returning clear CPT-level benefit summaries before services are delivered.
.avif)
Revenue Cycle Automation That Works With Your Current Tools
Fuse fits into your existing workflow with no new software to install or platform switch required. After a short onboarding call, practices can start using automated intake and insurance verification immediately with minimal disruption.
.avif)
After a short onboarding call, we start learning your existing workflows and customize our solution to minimize disruption to your team.
Why Transparent Healthcare Costs Matter Today
Three out of four patients worry about not being able to afford care. Surprise bills and unexpected costs are a top concern. Help reduce uncertainty and empower patients to make better decisions with transparent cost information.
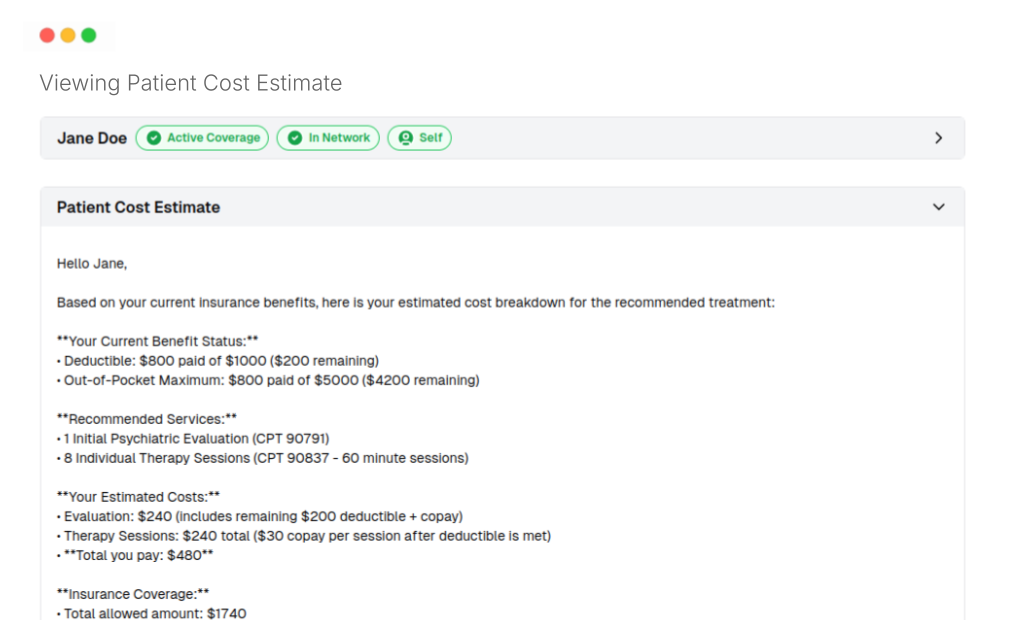
Patient Cost Estimator Tool with Real Numbers
Fuse calculates exact out-of-pocket costs for every visit using CPT-level insurance checks. Unlike vague estimator tools, patients can see a detailed breakdown of their treatment costs before they arrive.
.png)
Breaking Down Deductibles and Out-of-Pocket Costs
Terms like deductible, copay, and coinsurance often cause confusion. Fuse’s estimator tool clearly separates each element, so patients understand their financial responsibility in advance.
.png)
Prevent Underpayments and Improve Collections
Accurate, upfront estimates help practices collect more at the time of service and cut down on late payments. Fewer billing surprises mean better collection rates and a healthier revenue cycle.
.png)
This transparency improves the patient experience and makes financial conversations easier for staff. Practices that provide clear estimates upfront see fewer billing disputes and stronger collections, especially for higher-cost services.
This end-to-end process is extremely time-consuming for most clinics when done manually. Fuse integrates it into one connected workflow. Intake is also available at no cost to clinics using Fuse’s insurance verification, while many competitors charge up to hundreds of dollars per provider per month just for intake alone.
HIPAA-Compliant Healthcare Automation Platform


See Your Admin Time Drop in Weeks
The impact is visible quickly: fewer manual checks, faster verification, and cleaner front-end data flowing into billing. Schedule a demo to see the automation in action, hear the voice AI, and understand how Fuse can reduce administrative load while improving cash flow.

FAQs
What revenue cycle processes can Fuse automate?
Fuse automates front-end revenue cycle workflows including patient intake, insurance verification at the CPT level, payer portal checks, payer phone calls, and patient cost estimates.
How long does it take to implement revenue cycle automation?
Implementation is fast. Most practices can get started after a short onboarding call and begin using automated intake and insurance verification immediately.
How does Fuse’s intake integrate with insurance checks?
Patients enter insurance details directly into Fuse during intake. Fuse verifies the information, checks payer portals and calls payers when needed, then returns summarized CPT-level benefits without staff rework.
How does automated insurance verification improve accuracy?
Fuse combines real-time payer portal data with automated payer calls and AI summaries, ensuring eligibility and benefit details are confirmed before services are delivered.
What results can I expect from automating my revenue cycle?
Practices typically see reduced manual verification work, fewer eligibility-related denials, faster patient intake, and improved cash flow from clearer upfront pricing and cleaner front-end data.

